Let’s get one thing straight, we are not about portion control, counting calories, over exercising and restricting carbohydrates.
Seriously, we’re not about that life.
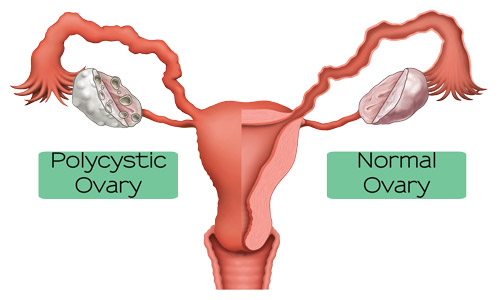
A diagnosis of polycystic ovary syndrome is a difficult one to hear especially when told that fundamental lifestyle changes are required. Fortunately, you definitely don’t need to throw your money at gym memberships, personal trainers, fancy yoga studios, and cookie-cutter low carb diet plans.
In this article we will cover a collection of tips we have compiled to help you start feeling your best and losing weight at the same time. PCOS is not necessarily a life sentence, a number of women have found a path to healing by adopting a moderate exercise routine as well as a high carb, low fat plant-based diet devoid of meat, dairy, eggs, oil and processed food.
If we have just added your primary food groups to the ‘no’ list, fear not. As a bonus, we have included a list of our favorite foods that promote weight loss, healthy blood glucose levels and prevent insulin resistance.
Eat Plants

Dr. Neal Barnard, founding president of the Physician’s Committee for Responsible Medicine, and his colleagues found in a comprehensive study that a low-fat, plant based whole food vegan lifestyle free of animal products and refined oils can help lower cholesterol, reduce blood pressure. Dr. Barnard further reports that this lifestyle aids in weight loss especially for individuals struggling with type 2 diabetes, a common concern for women with PCOS.
Whole foods like beans, lentils, legumes, oats, and rice are healthful and delicious staples to have. Fruits and vegetables like apples, bananas, pears, mangos, blueberries, blackberries, dates, spinach, garlic, broccoli, cauliflower, potatoes, and yams are also just a few of the healthiest foods a person can eat. When eaten daily and in abundance, these nutrient dense and antioxidant rich foods will change everything from your weight to the health of your skin and energy.
The variety of plant-based foods is astonishing. If you enjoy eating pizza, pasta and burgers, go ahead. There are plant-based pizzas loaded with tasty veggies, pastas made from rice, corn, peas and beets, and the best burgers you will ever taste made from beans, lentils, chickpeas, quinoa and so much more.
Mainstream media often curses some of these high-carb foods and recommends a diet rich in animal protein, especially for people struggling with PCOS. Unfortunately, you can’t trick your brain into wanting less food or fewer carbohydrates and women struggling with PCOS benefit immensely when foods like dairy, gluten, and soy are eliminated. These foods cause inflammation which can exacerbate symptoms of PCOS. By eating whole foods abundantly that are rich in carbohydrates, you will satisfy the cravings, flood your body with nutrients, feel amazing and lose weight.
No Oil
“From my lips to my hips, the fat you eat is the fat your wear,” said by Dr. McDougall, an American Physician and best-selling author.
The human body is incredibly efficient at storing fat. According to Dr. McDougall, the fats and oils found in both natural foods and added to foods, are among the leading causes of obesity.
If you cook with oil often, substituting with local, organic, fat-free oil, otherwise known as water, is incredibly easy.
Spice it up!

Whole foods can be healthy and satisfying. Discover the spices you love and add them to your favorite dishes. In fact, many spices deliver some serious health benefits. For example, a study conducted by the US Agricultural Research Service found that type 2 diabetics who consumed just 1 gram of cinnamon per day experienced a 20% decrease in blood sugar.
Other spices that pack punch not just in taste but in health benefits include turmeric, ginger, sage, red pepper, and cumin.
Get Adequate Sleep
This is always on our list of top weight loss tips and it should be on yours too.
The average person needs 7 to 9 hours of sleep per night for hormone balance and maintaining a healthy weight. In contrast, sleep deprivation can increase the production of certain hormones that increase feelings of hunger.
To get adequate sleep each night:
- Establish a routine beginning at least one hour before you go to bed that doesn’t involve any electronic devices.
- Keep your room as dark as possible. Even if you wear an eye mask, your body can sense light through your skin so try using black out curtains if necessary.
- Try to wake up and go to bed at the same time every day
Stop Resting
Not to be confused with ‘stop sleeping,’ a rather contradictory topic.
We mean stop resting for a day or days at a time between workouts. You can lower the intensity with walking, swimming, yoga with help from a free app or streaming video, or deep stretching. Practice moving everyday instead of lounging around on the couch on days where you haven’t scheduled cardio or weight training.
Life Weight, Lose Weight

Pay no attention to every time you have been told lifting weights will make you bulky and start building some fat-burning muscle. In fact, replacing ten pounds of fat with ten pounds of muscle can burn fifty more calories per day.
Performing exercises like squats and push-ups are also effective at building muscle and burning fat.
Love Yourself
No more fad diets, no more feeling guilty about sleeping in and no more hating yourself for eating. Losing weight, especially for people who have PCOS, is about long-term health. Quick fix low calorie, low carb diets and over exercising do not promote sustainable weight loss, long-term health and, most importantly, self love.
Love yourself enough to want to take care of your body. Your health is the priority and the physique you want is worth the wait.

We also recommend taking a high quality supplement. Furocyst, for example, is extracted from the Fenugreek seed without using chemicals and is rising in popularity as a beneficial supplement. Clinically proven safe and effective for managing PCOS, Furocyst is shown to reduce the size of ovarian cysts and improve insulin sensitivity. For more information, visit www.furocyst.com
The statement and product mentioned in this article have not been evaluated by the FDA to diagnose, treat, cure or prevent any disease.
or more,
Call : +91 9915002390
Click here
Losing Weight is Hard, Especially with PCOS. Here’s How We Can Help