Menstruation is part of every woman’s life. It involves vaginal bleeding that happens every month. This menstruation cycle takes place only in case when pregnancy does not occur and the lining of the uterus sheds in the form of blood as well as tissue particles through the vagina. These are the top 10 Things Each Woman Faces Every Month during Her Periods
It takes one month for the lining of the uterus (endometrium) to build up again in the form of tissue full of blood which is required for the implantation and growth of fertilized egg to be developed into the baby. But, this uterus lining sheds off from the uterus when no pregnancy occurs during that one month. This is known as the menstrual cycle.
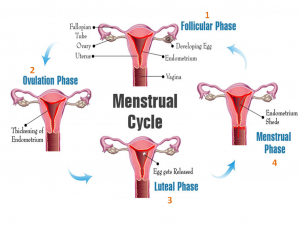
The menstruation cycle or periods start at the age between 11-14 years and stops at the age after 50 years (known as menopause). Generally, menstruation (or vaginal bleeding) occurs for 3-6 days and the number of days of the cycle varies from woman to woman according to the thickness of uterus lining. 10 Things Each Woman Faces Every Month during Her Periods
Besides the bleeding for at least 3-6 days every month, women also face many other problems during menstrual cycle or periods. Generally, these 10 Things Each Woman Faces Every Month during Her Periods are different according to the body composition of every woman but broadly these following given problems are the same.
- MOOD SWINGS
Mood swings or unaccountable change of mood is the most common problem during periods. These include irritation from the surrounding environment, instant anger, depressive state, sadness leading to crying, oversensitivity to every reaction from others and nervousness.
They are the outcome of the estrogen fluctuations during menstruation. 10 Things Each Woman Faces Every Month during Her Periods
Prevention strategy: Mood swings could be prevented during periods by following:
- Exercise can be very helpful for improving mood.
- Small and frequent meals can contribute to preventing mood swings.
- Avoid caffeine as much as possible as it can increase anxiety, nervousness, and insomnia.
- Try stress management exercises. Select permanent stress management exercises every time you face mood swings involving extreme sadness and crying.

- MENSTRUAL PAIN
Menstrual pain (or dysmenorrhea) is the major problem faced by the maximum number of females during the menstruation cycle. The body parts affected due to pain during menstruation include legs, lower tummy (belly) back and inner thighs. Menstrual pain occurs because of muscle contraction in the uterus.
Prevention strategy: The menstrual pain can be minimized during periods by the following strategies:
- Hot water bottle: Hot water bottle can provide extreme relief for the pain.
- Caffeine-containing food products should be avoided.
- Rest as much as possible.
- Pain reliever medications are also suggested in some cases when the pain becomes unbearable. These medications should only be consumed after consultation and prescription by the doctor.
- IRREGULAR APPETITE

Some of the women also experience loss of appetite or extremely high appetite during their menstrual cycle. It has been observed that the fluctuations in progesterone and estrogen in the brain influence the capability of females to under eating as well as over consume food.
Prevention strategy: The irregular appetite during the menstrual cycle can be controlled by managing food intake. The food to be consumed for the whole day should be properly noted and consumed accordingly instead of craving for food. This will help manage irregularity in food intake as well as solve weight loss or weight gain problems.
- HEADACHE, NAUSEA & VOMITING

These three problems in the menstrual cycle are associated with each other. Headache is the most commonly observed problem in women during their periods. Headache is associated with menstrual pain, heavy bleeding or low bleeding and lesser food intake too. These problems give rise to extreme headache. When headache persists then it gives rise to vomiting and nausea.
The instant decrease in estrogen and progesterone just before periods triggers headache which is known as menstrual migraine. 10 Things Each Woman Faces Every Month during Her Periods
Prevention strategy: This condition can only be prevented by prescription pain-killer medicines. Such medicines can also provide relief from menstrual pain. These pain-killers medicines help you get sound sleep to avoid the feeling of nausea and vomiting.
- DISTURBED STOMACH FROM LOOSE MOTION

This problem is a part of premenstrual syndrome in the major female population. Some females experience loose motions 1-2 days before their periods every month.
During the monthly cycle, cells of the uterus lining produce prostaglandins to help form the lining. The excess of prostaglandins causes loose motion by stimulating the large intestines and bowels to contract and expel their contents.
Prevention strategy: There is no such prevention strategy for this. As the periods take place, the lining of the uterus starts shedding expelling the cells as well as prostaglandins, relieving the body from loose motions as well.
If excessive loose motions take place, then, the doctor can be consulted for this who will prescribe medicine for this problem.
Heavy bleeding or menorrhagia during the menstrual period is also faced by some females. Bleeding during periods is considered as heavy if it is affecting normal life and causing severe problems such as extreme weakness and drop in hemoglobin. If you face the following problems, then, it is regarded as menorrhagia:
- Regularly experience flooding, when blood leaks on to your clothes or bedclothes.
- Clots are passed during bleeding.
- Feel the requirement of double sanitary protection.
- Feel restrictions in normal lifestyle due to heavy bleeding.
- BLOOD PRESSURE FLUCTUATIONS

It is normal in the menstrual cycle that the blood pressure fluctuations take place. Females generally face high blood pressure as premenstrual syndrome and face a sudden drop in blood pressure during the menstruation. This pattern of fluctuating blood pressure is due to the fluctuations in the hormonal profile.
Generally, the fluctuation in blood pressure is harmless unless the female is already a patient of blood pressure.
Prevention strategy: Drinking more water and staying hydrated during menstruation may help normalize the blood pressure. For females who are already on a prescription for their blood pressure should regularly check their blood pressure and take their medicine regularly on time, otherwise, it can become dangerous.
- FATIGUE
Tiredness and fatigue are common problems of premenstrual syndrome. Sleep problems, menstrual pain, and other above-mentioned problems combine to cause tiredness and fatigue in the body.
Prevention strategy: Tiredness and fatigue will remain until your period prolongs. It can be reduced to some extent by the following strategies:
- Keep your energy levels up by eating sufficient and nutritious food.
- Drink water to keep yourself hydrated instead of drinking coffee or juices.
- Avoid the consumption of alcohol.
- Exercise regularly such as brisk walking to provide energy to your body.
- TROUBLE SLEEPING & CONCENTRATING
Trouble to sleep is most commonly observed in those women who experience extreme menstrual pain, irregular appetite, an increase in body temperature during periods. It also interferes with your power to concentrate well for conducting day-to-day activities. 10 Things Each Woman Faces Every Month during Her Periods
Prevention strategy: The sleeping disturbance and concentration problem can be resolved by the following strategies:
- Take a warm bath before going to sleep. It can help to control menstrual pain as well as make it easy to sleep well.
- Avoid eating just before sleeping as it will not help you to sleep on time.
- Mind and body relaxation techniques such as deep breathing and yoga help you get sound sleep by relaxing your body and mind during periods.
- Avoid sleeping in the afternoon or evening.
- BLOATED AND PAINFUL BREAST

Bloated and painful breasts are the sign of the premenstrual syndrome. The pain is usually severe just before the menstrual cycle and reduces periodically as the days of the menstrual cycle ends.
Hormonal levels are the reason behind breast pain and extreme fluctuations can worsen breast pain.
Prevention strategy: It is recommended that the breast pain diminishes as the menstrual day’s end. If the pain persists even after periods, then, you should consult the doctor.
Consult your health care provider if you have big changes during your cycle. They may be the signs of other problems that should be treated. If you experience irregularity in the menstrual cycle, then, the above-given problems can worsen. In that case, it is better to consume herbal medications which will also be safe under this problem.
In that case, it is better to consume herbal medications which will also be safe under this problem.
One such herb is Furocyst® made from fenugreek seeds, which is even clinically-proven to help maintain regularity in the menstrual cycle. Furocyst named fenugreek seed extract-based supplement is clinically proven to safely maintain the regularity in the menstrual cycle to get relief from menstrual problems.
REFERENCES
- https://medlineplus.gov/menstruation.html
- http://natural-fertility-info.com/thin-lining-of-the-uterus-build-the-uterine-lining-naturally.html
- https://www.everydayhealth.com/pms/mood-swings.aspx
- http://www.webmd.com/women/menstrual-cramps#1
- https://academic.oup.com/humrep/article/12/6/1142/573355/Menstrual-cycle-and-appetite-control-implications
- http://www.webmd.com/migraines-headaches/guide/hormones-headaches#1
- http://goaskalice.columbia.edu/answered-questions/monthly-diarrhea-%E2%80%94-associated-my-period
- http://vascuvite.com/high-blood-pressure-during-period/
- http://www.livestrong.com/article/93433-overcome-extreme-fatigue-during-menstruation/
- https://sleepfoundation.org/sleep-news/6-sleep-problems-occur-during-your-period-and-what-do-make-them-go-away





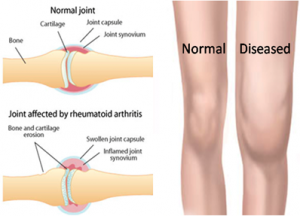


 Being active is one of the best things you can do for yourself, even if you have rheumatoid arthritis. You just have to know how to work within your limits because too much exercising involving stress on the joints can be harmful.
Being active is one of the best things you can do for yourself, even if you have rheumatoid arthritis. You just have to know how to work within your limits because too much exercising involving stress on the joints can be harmful.
 Managing inflammation is a key component to living with rheumatoid arthritis (RA). This chronic condition results in the immune system attacking the joints, causing inflammation and pain.
Managing inflammation is a key component to living with rheumatoid arthritis (RA). This chronic condition results in the immune system attacking the joints, causing inflammation and pain.
 It has been reported that fenugreek is an effective remedy to treat
It has been reported that fenugreek is an effective remedy to treat







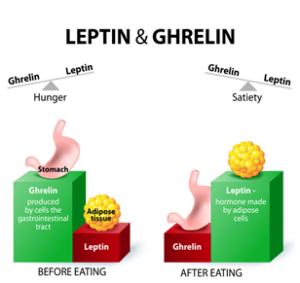
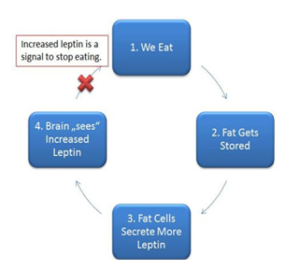
 Leptin
Leptin





