We have organised the CME meet on Furocyst – For PCOS MANAGEMENT on 22nd February ,2016 at Barbecue Nation Sector 26, CHANDIGARH. Speaker, Dr Ruchi Rai Ahuja, Senior Consultant At Paras Bliss, MDC, Panchkula shared the knowledge about PCOS & benefit of furocyst in PCOS. 

Year: 2017
Free Blood Sugar Check-up Camp in Tricity

Team FENFURO in association with Dabur Dhanvantry Hospital had organised a free Blood Sugar check-up & awareness camp for general public on 25th February, 2017 at Dabur Dhanvantry Hospital, Sector-46B, Chandigarh. Patients who was identified with high blood sugar level was referred to the hospital for further opinion from the doctor and treatment.
Team FENFURO had organised this camp to create awareness regarding the causes, prevention and Management of Diabetes under the Niyantrit Madhumeh Bharat campaign supported by the Ministry of Ayush.
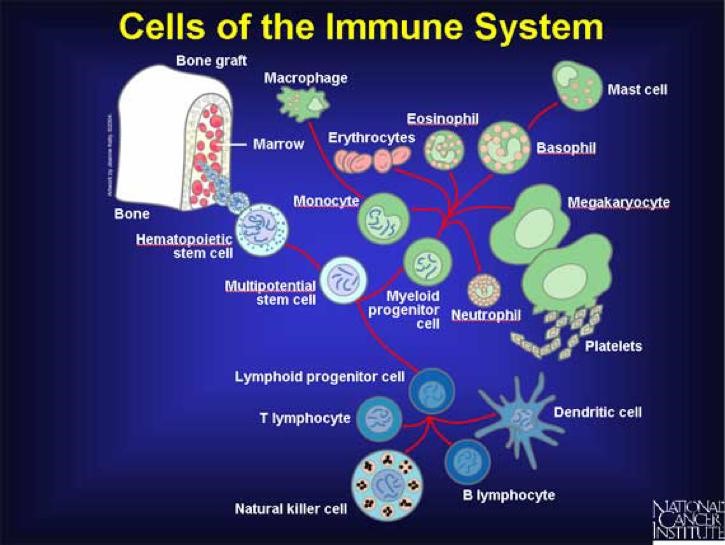
A major function of the immune system is to recognize foreign objects (viruses, bacteria, parasites, splinters, and anything else that isn’t supposed to be in your body) and destroy them. Immune cells do this by recognizing specific targets on the surface of the item to be destroyed. Cancer cells are abnormal and may be recognized as ‘foreign’ by immune cells. Immune cells recognize small molecular ‘flags’ associated with tumor cells (called tumor specific antigens (TSAs) or tumor associated antigens (TAAs)). Immune cells can then kill these cancer cells.
Note: An antigen can be defined as anything the immune system can recognize. It is a general term. Antigens can be proteins, sugars, lipids, nucleic acids, or hybrid molecules. Most antigens are proteins.
 If the immune system is able to recognize and kill cancer cells, why do people get cancer?
If the immune system is able to recognize and kill cancer cells, why do people get cancer?
It is thought that most cancers are caught very early and eliminated by the immune system. The cancers that survive have to be able to evade the immune system. It turns out that there are several ways that cancer cells avoid being recognized and killed. These include:
- Cancer cells form from normal cells. Because cancer arises from a person’s own cells, it’s trickier for the immune system to recognize cancer cells than to identify a truly foreign invader like a virus.
- Cancer cells with the most targets on them are most easily killed by the immune system. This sounds like a good thing, and it can make tumors shrink, but after a while, the cancer cells that are left have less targets on their surface. Those with the least amount of target antigens on their surface have the best chance of surviving, and tend to take over, making the cancer resistant to immune cells. It is similar to treating a lawn with weed killer. Any weeds that are resistant will survive and grow. After that, the weed killer will not work anymore. The immune system accidentally ‘selects’ for cancer cells that it can’t recognize.
- Cancer cells can hijack normal control systems to turn the immune system ‘off’ in and around the tumor. To keep the immune system under control, there are several controls (like ‘on-off’ switches) that work to regulate the activity of immune cells. Some cancer cells are able to flip that switch, turning the immune system off in the area around and in the tumor. Treatments designed to reverse this are very promising and are described more below.
- Cancer cells can evade the immune system by making less of the ‘self’ signals that immune cells use to recognize defective or infected cells.Cancer proteins can be shown to the immune system by being stuck to cellular versions of flagpoles. By taking down the poles, cancer cells prevent this from happening and are able to avoid being recognized and killed.
Refernce:
- Vinay DS, Ryan EP, Pawelec G, Talib WH, Stagg J, Elkord E, Lichtor T, Decker WK, Whelan RL, Kumara HM, Signori E, Honoki K, Georgakilas AG, Amin A, Helferich WG, Boosani CS, Guha G, Ciriolo MR, Chen S, Mohammed SI, Azmi AS, Keith WN, Bilsland A, Bhakta D, Halicka D, Fujii H, Aquilano K, Ashraf SS, Nowsheen S, Yang X, Choi BK, Kwon BS. Immune evasion in cancer: Mechanistic basis and therapeutic strategies. Semin Cancer Biol. 2015 Mar 25. pii: S1044-579X(15)00019-X [Epub ahead of print] [PUBMED]
- Seliger B. Strategies of tumor immune evasion. BioDrugs. 2005;19(6):347-54. [PUBMED]
- Poggi A, Musso A, Dapino I, Zocchi MR. Mechanisms of tumor escape from immune system: role of mesenchymal stromal cells. Immunol Lett. 2014 May-Jun;159(1-2):55-72. Epub 2014 Mar 20. [PUBMED]

PCOS (Poly cystic ovary syndrome) is a disease involving the development of multiple cysts in the ovaries. Its global prevalence is increasing day by day due to the development of multiple complications along with it. The complications originated by PCOS involve infertility, hirsutism, skin problems, insulin resistance, cardiovascular health risk, etc.
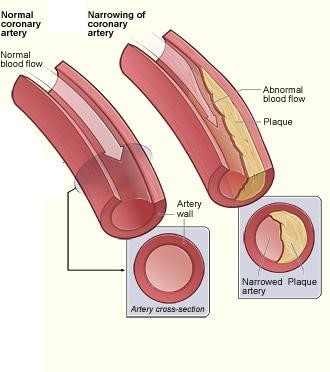
It is reported that women with PCOS are nearly twice as likely to suffer from atherosclerosis (plaque deposits in the arteries), than women without the syndrome. Atherosclerosis sharply increases the risk of coronary heart disease and stroke.
REASON FOR DEVELOPMENT OF PCOS
The underlying causes of PCOS in women are:
- Insulin resistance
- Hormonal imbalance
- Elevated levels of LDL “bad” cholesterol
- High blood pressure
- Obesity
REASON FOR DEVELOPMENT OF CARDIOVASCULAR DISEASE IN PCOS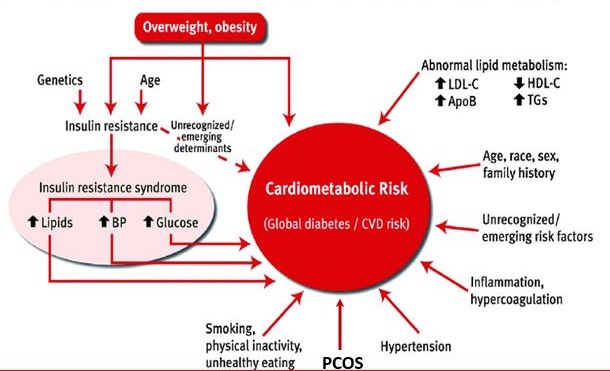
Numerous studies have found that PCOS put the sufferers at higher risk of developing future serious, life-threatening health conditions such as coronary heart disease and stroke due to:
- High blood pressure
- Hypertension
- Excessive fat tissue in and around the abdominal area
- Blood fat disorders (high triglycerides and low HDL)
- Hyper-androgenism (elevated levels of male hormones)
- Insulin Resistance
DEVELOPMENT OF CARDIOVASCULAR DISEASE UNDER THE INFLUENCE OF “INSULIN RESISTANCE” IN PCOS
Insulin is produced in the pancreas and released into the circulatory system where it is the key to the absorption of glucose by the cells. If the cells resist insulin, both insulin and glucose build up in the blood. Excess insulin leads to weight gain and high blood pressure. As insulin comes in contact with the interior wall of the arteries, it damages the tissue, causing the initial injury that produces plaque. Therefore, having both insulin resistance and PCOS directly causes negative changes in the blood lipids and overall cardiovascular health.
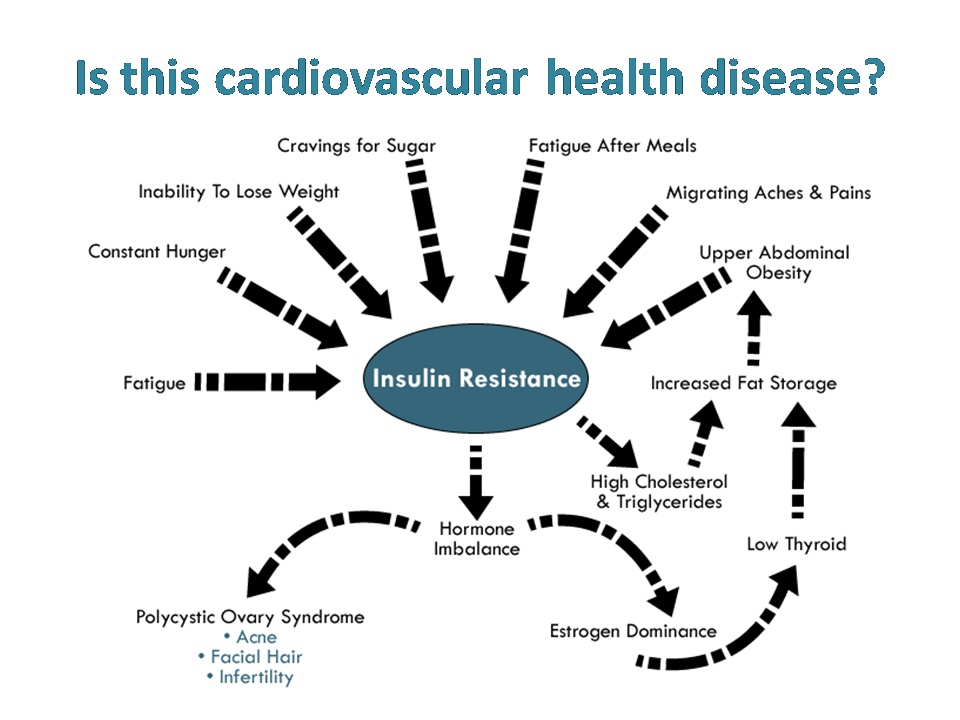
This is due to the higher levels of insulin that have been associated with PCOS and are known to increase one’s risk for elevated triglycerides, low levels of high density lipoprotein (HDL), high cholesterol, blood pressure and atherosclerosis. These conditions can increase the risk for a heart attack and stroke.
RECOMMENDATIONS FOR REDUCING THE RISK OF HEART DISEASE
- Blood pressure & cholesterol: The first step to reduce the risk of cardiovascular health is to have the blood pressure and cholesterol levels checked routinely and talk to the doctor about the risk factors.

- Dietary modification: The most important thing which can be done is to maintain a healthy weight through diet and exercise. This can be done through careful food choices.
Reducing the intake of saturated fat and salt is important. Sources of saturated fat typically include animal products such as red meat, processed poultry and butter. Instead, replace saturated fat with unsaturated sources of fat such as olive oil, nuts, seeds, and avocados.
Eating a diet rich in fruits and vegetables, which contain fiber and phytonutrients, is also helpful. Additionally, including 2 grams each day of plant stanols has been shown to reduce the risk for cardiovascular disease.
The more body fat that you have and the more you weigh, the more likely you are to develop coronary heart disease. Losing weight and increasing physical activity work together to reduce the risk for cardiovascular disease. Especially in overweight women, weight loss is a major parameter for treating PCOS along with reducing the risk of cardiovascular health.
Loss of just 3 to 5% of current body weight can lower triglycerides and glucose levels in the blood, as well as the risk of developing type 2 diabetes. A 3 to 5% body weight loss also can improve blood pressure readings, lower bad LDL cholesterol and increase good HDL cholesterol.
- Manage stress:
 Hypertension is a major contributor in both PCOS and cardiovascular health risk. Emotionally upsetting event, particularly anger, can serve as a trigger for the heart attack or angina in some people. This can contribute to high blood pressure and thus, cardiovascular health risk. Consider healthy stress-reducing activities such as
Hypertension is a major contributor in both PCOS and cardiovascular health risk. Emotionally upsetting event, particularly anger, can serve as a trigger for the heart attack or angina in some people. This can contribute to high blood pressure and thus, cardiovascular health risk. Consider healthy stress-reducing activities such as - Visiting a qualified mental healthcare provider
- Participating in a stress management program
- Practicing meditation
- Being physically active
- Trying relaxation therapy
- Talking with friends, family, and community or religious support systems
-
Medication:
Sometimes lifestyle changes are not enough to control the blood cholesterol levels.

For managing cardiovascular health risk
You may need statin medications to control or lower the cholesterol. By lowering cholesterol levels, you can decrease the chance of having a heart attack or stroke.
For managing PCOS
- Combinationestrogen and progestin hormones in birth control pills, vaginal rings, or skin
- Androgen-loweringspironolactone, which is a It is often used with estrogen-progestin therapy reducing hair loss, acne and abnormal hair growth on the face and body (hirsutism).
- Insulin sensitizer drugs for controlling insulin, blood sugar levels and androgen levels.
- Clomiphene (Clomid,Serophene) (fertility medicines) and gonadotropin injections (LH and FSH).
- Herbal treatment including clinically proven therapy for PCOS e. fenugreek seed extract – as Furocyst®
REFERENCES
- https://pcos.com/pcos-and-heart-disease-what-are-the-implications/
- https://www.verywell.com/pcos-and-heart-disease-2616320
- http://jcp.bmj.com/content/58/2/151.full
- https://www.nhlbi.nih.gov/health/health-topics/topics/cad
- https://www.nhlbi.nih.gov/health/health-topics/topics/heart-healthy-lifestyle-changes/aiming-for-a-healthy-weight
- http://www.webmd.com/women/tc/polycystic-ovary-syndrome-pcos-medications

Our company has been awarded ‘AIMA – Dr. J S Juneja’ for Creativity and Innovation for Micro Small & Medium Enterprises, 2016 by Dr. J S Juneja, Past President of AIMA and Former Chairman.
STRUGGLING WITH JOINT PAIN IN PCOS
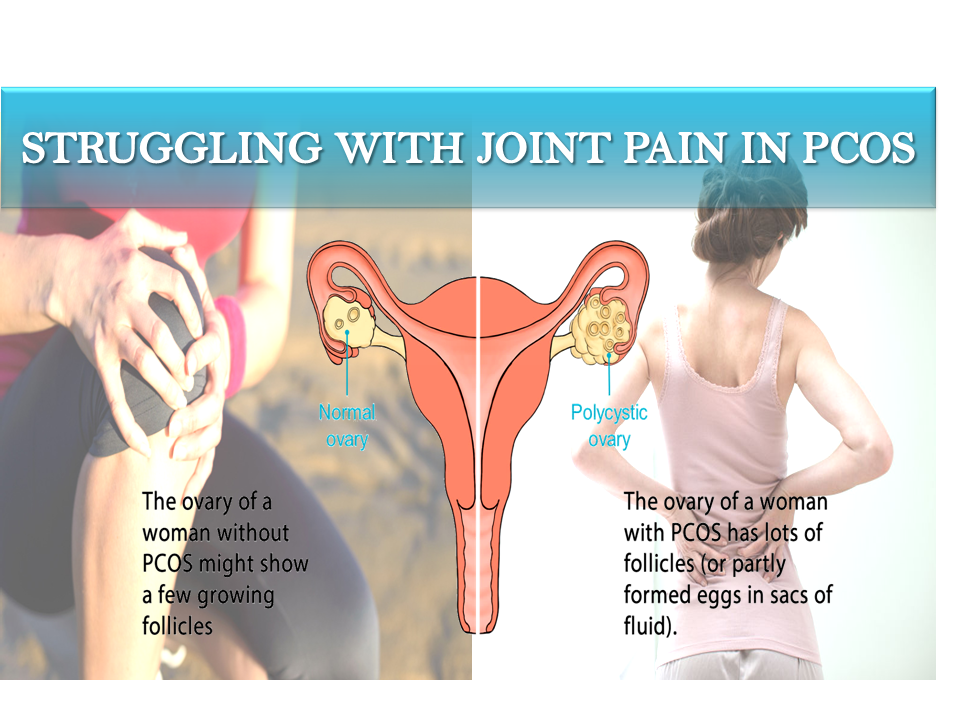
POLYCYSTIC OVARY SYNDROME is one of the most common diseases among women of childbearing age and cause of infertility. There are over 5 million affected women in the US and 105 million worldwide who are suffering from PCOS.
Another disease i.e. RHEUMATOID ARTHRITIS is a chronic progressive disease causing inflammation in the joints. It has been found that PCOS also gives rise to this rheumatoid arthritis in women. Joint pain and rheumatoid arthritis (RA) generally develops in old age due to the weakening of immune system of the body. But it has been confirmed by scientific studies that women with PCOS having irregular menses or a truncated menstrual history (e.g., early menopause) have an increased risk of RA.
In reverse, the inflammation originated from rheumatoid arthritis worsens the condition of PCOS because somehow, the chronic low grade inflammation from RA has been linked to insulin resistance. If the insulin levels are higher than they should be, the ovaries start to produce too much testosterone, which makes PCOS even worse.
HOW PCOS AND RHEUMATOID ARTHRITIS LINKED?
The immune system is influenced by signals from the female reproductive hormones. It seems that the levels of hormones, such as estrogen and testosterone, as well as changes in these levels can promote autoimmunity. “Autoimmunity” is a condition whereby the immune system (which normally wards off foreign invaders of the body, such as infections) turns and attacks the body’s own tissues, such as skin, joints, liver, lungs, etc. Autoimmune diseases typically feature inflammation of various tissues of the body.
It is known that hormones play major role in the development of rheumatoid arthritis. It is also known that PCOS is that syndrome which involves the imbalance of the reproductive hormones. Disturbance in these hormones such as progesterone & estrogen, gives rise to rheumatoid arthritis.
SYMPTOMS OF RHEUMATOID ARTHRITIS
 Tender, warm, swollen joints
Tender, warm, swollen joints- Joint stiffness that is usually worse in the mornings and after inactivity
- Fatigue, fever and weight loss
Early rheumatoid arthritis tends to affect the smaller joints first – particularly the joints that attach fingers to the hands and toes to the feet.
As the disease progresses, symptoms often spread to the wrists, knees, ankles, elbows, hips and shoulders. In most cases, symptoms occur in the same joints on both sides of your body.
DIAGNOSIS

- Rheumatoid arthritis in PCOS can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis.
- Physical examination
During the physical exam, the doctor will check the joints for swelling, redness and warmth. Doctor may also check the reflexes and muscle strength.
- Blood tests
People with rheumatoid arthritis often have an elevated erythrocyte sedimentation rate (ESR, or SED rate) or C-reactive protein (CRP), which may indicate the presence of an inflammatory process in the body. Other common blood tests look for rheumatoid factor and anti-CCP antibodies.
- Imaging tests
Doctor may recommend X-rays to help track the progression of rheumatoid arthritis in the joints over time. MRI and ultrasound tests can help doctor judge the severity of the disease in body.
COMPLICATIONS OF RA
§ Lung disease
§ Heart problems
§ Nerve damage
§ Osteoporosis
§ Eye complications such as dry eye syndrome
PREVENTION AND TREATMENT
- Meal planning

There are many foods that can help to reduce inflammation originated from RA inside the body. Eating a wide variety of whole foods is the key to reduce inflammation. The plant-based foods rich in vitamins and nutrients that target inflammation include:
- Fruits
- Vegetables
- Beans
- Nuts
- Seeds
- Whole grains
- Turmeric
Some foods are extremely beneficial to reduce inflammation. Often, fruits and vegetables contain antioxidants, which combat inflammation. Antioxidants are found in very colorful foods, such as berries, and dark and leafy greens, and these help support the immune system. Turmeric Curcumin is also a great source to reduce inflammation.
Eating inflammatory foods should be avoided. Some of these foods include:
- Deep-fried foods
- Processed food
- Red meat
- Sugary drinks
- Refined grains, such as those found in white bread
- Exercise

Being active is one of the best things you can do for yourself, even if you have rheumatoid arthritis. You just have to know how to work within your limits because too much exercising involving stress on the joints can be harmful.
Fitness as a regular part of the life provides many benefits for PCOS as well as RA patients such as:
- Less pain fromrheumatoid arthritis.
- Stronger bones. This is important because RA can thin your bones, especially if you take
- You’ll move better and have more energy.
- It’s good for yourheart and all your other muscles.
- It helps to lose body weight in obese women
- It helps to control diabetes
Exercises such as low-impact activities, like walking, swimming, bicycling, or using an elliptical machine could be beneficial to manage rheumatoid arthritis. Any of these will get the heart pumping.
Be careful about activities that put a lot of stress on a joint, or are “high-impact,” such as:
- Jogging, especially on paved roads
- Heavyweight lifting
- Balancing hormones
Maintaining normal levels of the reproductive hormones estrogen and progesterone appear to have a protective effect against both RA and PCOS. The medications given in following section can be effective at balancing hormones.
- Medication

Managing inflammation is a key component to living with rheumatoid arthritis (RA). This chronic condition results in the immune system attacking the joints, causing inflammation and pain.
- Medications used in the treatment of rheumatoid arthritis include NSAIDs, DMARDs, TNF α-inhibitors, IL-6 inhibitors, T-cell activation inhibitors, B-cell depleters, JAK inhibitors, immuno suppressants and steroids.
- The contraceptive pill may be recommended to induce regular periods, or periods may be induced using an intermittent course of progestogen tablets (which are usually given every three to four months, but can be given monthly).
- A medication called clomifene is usually the first treatment recommended for women with PCOS who are trying to get pregnant. Clomifene encourages the monthly release of an egg from the ovaries (ovulation).
- Clinically proven herbal remedy for PCOS including fenugreek seeds extract (Furocyst) can also be prescribed due to its great effectiveness in the PCOS patients.
REFERENCES
- http://www.medicina-interna.ro/articol.php?articol=635
- https://www.cdc.gov/arthritis/basics/rheumatoid.htm
- http://www.pcosdietsupport.com/pcos-symptoms/pcos-and-inflammation/
- http://www.ehealthme.com/cs/rheumatoid%20arthritis/pcos/
- http://www.healthline.com/health/rheumatoid-arthritis/hormone-imbalance#2
- https://www.ncbi.nlm.nih.gov/pubmed/6859063
- http://www.semarthritisrheumatism.com/article/S0049-0172(02)70110-8/pdf
- http://www.everydayhealth.com/hs/guide-to-managing-ra/signs-of-complications/
- http://www.healthline.com/health/rheumatoid-arthritis/seasonal-foods-ra#Spring3
- http://www.webmd.com/rheumatoid-arthritis/guide/exercise-and-rheumatoid-arthritis
- http://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/diagnosis-treatment/diagnosis/dxc-20197396
- http://www.medicinenet.com/script/main/art.asp?articlekey=13186
ERECTILE DYSFUNCTION (ED) is a common medical disorder which decreases the quality of life in men. Its prevalence is increasing worldwide with estimated 322 million cases by the year 2025.
Risk factors associated with erectile dysfunction which are modifiable include
- Smoking
- Lack of physical activity
- Poor diet
- Overweight or obesity
- Metabolic syndrome such as diabetes, cardiovascular disease, etc
- Excessive alcohol consumption
- Stress
- Psychological issues
Medical conditions are a frequent cause of erectile dysfunction. But sometimes, the cause may be related to lifestyle choices. It has been suggested that lifestyle habits have a critical role in reducing the burden of sexual dysfunction.
Both basic and clinical studies have shown that targeting several lifestyle factors commonly associated with ED, such as smoking, alcohol consumption, obesity and limited physical activity can have significant effects on improvement of erectile function as well as testosterone levels.
HOW UNHEALTHY LIFESTYLE COULD BE A CONTRIBUTOR IN WORSENING ED?

Lifestyle and nutrition have been recognized as central factors influencing both vascular nitric oxide (NO) production and erectile function. Unhealthy lifestyle is strongly associated with conditions that result in endothelial dysfunction by decreasing the availability of nitric oxide (NO), which is mandatory for the genital blood flow. Changes in lifestyle and nutrition can influence vascular NO production, testosterone levels and thus, erectile function. Therefore, maximal attention should have to be paid on measures known to increase vascular NO production. The promotion of healthy lifestyle would yield great benefits in reducing the burden of sexual dysfunction by increasing vascular NO production.
PREVENTION & TREATMENT OF ERECTILE DYSFUNCTION
As with many other medical diseases, prevention may be the most effective approach to alleviate the consequences of ED. Despite the increasing evidence that unhealthy lifestyles lead to metabolic diseases, including sexual dysfunction, the majority of adults fail to meet physical activity and nutritional guidelines. There are some approaches related to lifestyle changes which have been given below to improve erectile dysfunction:
- Physical activity

How is it effective?
The mechanisms by which physical activity ameliorates ED include improved cardiovascular fitness and endothelial dysfunction, increase in endothelial-derived NO, decrease in oxidative stress and increase in regenerative cells. Moreover, physical exercise showed beneficial effects on self-esteem and mental health, with a positive impact on psychological issues associated with sexual dysfunction.
Recommendation: It is recommended that adults following 30 minutes of moderate to intense aerobic physical activity on most days of the week will benefit greatly from erectile dysfunction. Exercise helps to reduce stress and increase energy levels. It also improves circulation and helps to keep the arteries and heart healthy.
- Weight loss

How is it effective?
Increased abdominal fat and related risk factors are associated with decrease in the availability and activity of NO. The reduced testosterone levels associated with obesity and the metabolic syndrome may worsen both insulin resistance and endothelial function, thereby contributing to ED. Body weight loss is associated with decline in estrogen levels and rise in gonadotropins and testosterone (hormones), which increases consecutively with weight loss.
Recommendation: Weight loss of 5%–10% in overweight or obese non-diabetic or diabetic men can result in effective improvement in erectile function in a short period. Regular exercise without any gap can result in effective weight loss and thus, improving erectile dysfunction.
- Dietary factors

How is it effective?
The abundant consumption of vegetables, fruit and whole grain and the dietary patterns rich in these foods produce a markedly lower risk of coronary disease. The beneficial effect of the Mediterranean diet on atherosclerosis and ED can be mediated through multiple biological pathways, including the reduction of oxidative stress and subclinical inflammation, amelioration of endothelial dysfunction and insulin sensitivity, which in turn may increase NO release in the penile arteries.
Recommendation: Mediterranean diet has been proposed as a healthy dietary pattern based on the evidence that greater adherence to this diet is associated with lower all-cause and disease-specific survival. Diet rich in fruits & vegetables but devoid of high sugar as well as fat can be effective in improving erectile dysfunction.
- Smoking

How is it a contributor?
Both the direct use of tobacco and second-hand exposure seems to be a risk factor for ED due to the effects of cigarette chemicals on the blood vessels in the penis.
Recommendation: Quitting smoking can improve ED symptoms. If it seems to be difficult to quit smoking, seek help from medical practitioners.
How is it effective?
Alcohol is a depressant and using it heavily can dampen mood, decrease sexual desire and make it difficult for a man to achieve erections while under the influence.
Recommendation: Most experts say moderation is the key. According to the U.S. Centers for Disease Control and Prevention (CDC), moderate drinking, no more than two drinks a day for men, will not give rise to erectile dysfunction.
NATURAL REMEDIES FOR ED

Along with lifestyle changes, there are natural remedies available for the treatment of ED. The following are some supplements that have been studied and shown to be safe. They may also be effective in the treatment of ED.
- DHEA
- Ginseng
- L-arginine
- Fenugreek seed extract – in the supplemental form e. Chemforce.
WHEN SHOULD YOU SEE A DOCTOR FOR ERECTILE DYSFUNCTION SYMPTOMS? 
Erectile dysfunction can be troubling and affect sexual and psychological health. If you are experiencing erectile dysfunction symptoms, you should examine your diet, try to work towards a healthy weight and seek the guidance of a doctor before starting any medical or supplement treatment. You should especially see a doctor if you have known heart disease, or other vascular disease (such as in the legs) because ED can be a sign of worsening vascular disease.
REFERENCES
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4291878/
- http://www.webmd.com/erectile-dysfunction/news/20110913/lifestyle-changes-may-improve-erectile-dysfunction
- http://www.ajandrology.com/article.asp?issn=1008-682X;year=2015;volume=17;issue=1;spage=5;epage=10;aulast=Maiorino
- http://www.healthline.com/health/type-2-diabetes-lifestyle-factors-and-erectile-dysfunction
- http://www.everydayhealth.com/erectile-dysfunction/why-boozing-can-be-bad-for-your-sex-life.aspx

Nowadays, diabetes, particularly type 2 diabetes, is one of the fastest growing chronic diseases in the society. Tight blood glucose control, dietary requirements and intake of regular medication are only few things that a diabetic patient needs to manage in order to prevent long-term complications. Assured continuity of care does not only create many challenges for the patient but also for the treating physician who will need to support the patient’s management strategies.
PATIENT EMPOWERMENT refers to a process that enables and facilitates behavior change. The key to empowerment does not necessarily means better compliance to what the doctor says or prescribes but rather in the opportunity to increase patients’ self-sufficiency to improve their decision-making capabilities.
Research has shown that diabetes education is central to effective self-management behavior, which in the long term can influence clinical and psychological outcomes.
Approaches have now moved from purely educational interventions to those that empower patients based on the assumption that they are managers of their own health. Diabetes education together with patient empowerment has shown to be the key for effective self-management behavior. When delivered through information and communication technologies (ICT), this solution has shown to lead to better health outcomes.
KEY ELEMENTS OF EMPOWERMENT

- Diabetes awareness
- Education & training
- Support of healthcare providers
CHARACTERISTICS OF AN EMPOWERED ACTIVATED PATIENT

- He understands his health condition and its effect on his body.
- He feels able to participate in decision-making with his healthcare professionals.
- He actively seeks out, evaluates and makes use of information.
- He feels able to make informed choices about treatment.
- He is able to challenge and ask questions of the healthcare professionals providing their care.
- He takes responsibility for his health and actively seeks care only when necessary.
- He understands the need to make necessary changes to his lifestyle for managing their conditions.
HOW TO EMPOWER PATIENTS?

- DIABETES EDUCATION
Diabetes education for the nurses is vital in forming solid knowledge that will equip them to be able to properly educate their patients.
Poor education not only reflects in poor health for the patient but also leads to serious complications and early death imposing a large economic burden on the individual and healthcare systems.
Benefit: This would reduce excess costs for emergency department care and care needed for complications concerning uncontrolled diabetes. A lot of the complications that diabetics face could be prevented easily.
There is a large amount in the community of diabetics that simply do not care about their nutrition or health and are unwilling to make any sort of lifestyle change, those people aside; there is no excuse for the overwhelming amount of complications that some diabetics suffer from due to the lack of knowledge.
A patient with uncontrolled diabetes deals with physical ailments; people with uncontrolled type 1 diabetes often feel ill, experience cognitive dysfunction, have difficulty maintaining their weight at a desired level, and experience fluctuating moods.
Diabetes education can greatly decrease hypoglycemic events in patients with diabetes.
- SELF MANAGEMENT
 Self-management is seen as a key capability for Patient Empowerment and emphasizes that persons with chronic diseases has the central role in managing their health.
Self-management is seen as a key capability for Patient Empowerment and emphasizes that persons with chronic diseases has the central role in managing their health.
Self-management is what people do to manage their diabetes or other chronic condition and its effects on their physical health, daily activities, social relationships and emotions.
Mindful eating: Mindful eating empowers the patient to make flexible decisions through the challenges of life. Mindful eating is one way to get closer to meeting the true needs and in the process gradually allows a person to live the life more fully.
Putting someone on a diet that says to avoid rice, “sweets”, “anything white” or “everything fried” automatically creates cravings and (even worse) guilt if they finally respond to their cravings. When a person gives into their cravings, the patient takes the wrong way & fails to manage diabetes.
- INTERNET
 Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.
Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.
The key issue for patients & healthcare professionals is how to deliver personalized behavioral support in ways that are affordable and can reach to maximum number of patients. The internet offers several advantages in this regard because it is available 24 hours a day with very low cost.
Benefits
- It does not require large investments.
- It does not imply high fees.
- It can easily be enriched with new information which immediately becomes available to the target group of users in any location in the world.
- Help patients to monitor their diet and medicinal doses
- Help both the patient and doctor to monitor the long term effect of the interventions
We cannot empower patients!
We only can provide a framework (tools, services, etc.) that makes it easier for patients to empower themselves.
REFERENCES
- http://www.idb.hr/diabetologia/02no1-1.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4372173/
- http://www.reaction-project.eu/downloads/clustering%20event/EMPOWER.pdf
- http://ceur-ws.org/Vol-532/paper11.pdf
- http://www.dnaindia.com/health/report-mindful-eating-empowering-patients-with-diabetes-to-take-charge-of-their-diet-2145200

UNHEALTHY LIFESTYLE factors such as alcohol consumption have major impact on the severity of erectile dysfunction in men. It is long regarded as a risk factor for erectile dysfunction. Alcohol consumption leads to marked distress and interpersonal difficulty in erectile deficient men. It has been found that 61% of patients dependent on alcohol suffer from sexual dysfunction, the most common being erectile dysfunction followed by reduced sexual desire. Erectile dysfunction and reduced sexual desire are frequently co-exist.
The scientific explanation is that alcohol is a central nervous system depressant. This causes impotence and other disturbances in sexual dysfunction. Erectile failure in alcoholic men is fairly a routine which is found to be higher in men consuming more than three standard units of alcohol (12 g ethanol) daily and in subjects smoking more than 10 cigarettes/day.
SYMPTOMS OF ALCOHOL-INDUCED ED
The symptoms of erectile dysfunction originated from alcohol consumption appeared accordingly with the amount of alcoholic beverage consumed. The chance of developing sexual dysfunction appears to increase with increasing quantity of alcohol consumed.
Higher levels of alcohol intake may result in greater neurotoxic effects. Heavy use of alcohol is also known to alter gonadal hormones (testosterone & follicle-stimulating hormone).
MECHANISM – BY WHICH ALCOHOL CAUSES ERECTILE DYSFUNCTION

In addition to the effect of alcohol on central nervous system receptors (as given above), alcohol also suppresses the release of gonadotropin and anti-diuretic hormone from the pituitary that may be associated with hypogonadism and hypovolemic shock in alcohol abusers. The chronic abuse of alcohol may cause testicular atrophy, inhibition of testosterone production and impairment of spermatogenesis, apart from its direct oxidative toxicity. These effects of alcohol cause erectile dysfunction because it directly affects the production of hormones responsible for erectile mechanism in males.
All this alcoholism effects are found to cause men to suffer from problems achieving and maintaining an erection, because alcohol can also prevent blood vessels in the penis from closing, inhibiting the ability of penis to remain erect. In a healthy, non-alcoholic man, the penis becomes erect when aroused because it fills with blood and the vessels close, preventing back-flow. Chronic consumption of alcohol damages blood vessels which cause problems in the heart and also in the penis.
EXAMINATION
- Physical examination

- Genitourinary examination
- Attention to any endocrine (including testicular size and secondary sexual characteristics), neurological or vascular causes as appropriate, especially if indicated by the history.
- Pulse (including peripheral pulses) and blood pressure. Because ED shares risk factors with CVD, a full cardiovascular assessment should be performed.
- Rectal examination in patients over the age of 50 years.
- Psychological counseling involving queries regarding stress, depression or alcohol consumption
- Laboratory examination

- Fasting glucose
- HbA1c
- lipid profile
- Total testosterone
- Follicle-stimulating hormone (FSH), luteinising hormone (LH), and prolactin when low testosterone is detected
MANAGEMENT OF ERECTILE DYSFUNCTION

When you drink heavily and frequently, your body becomes physically dependent on alcohol and goes through withdrawal if you suddenly stop drinking. The symptoms of alcohol withdrawal range from mild to severe, and include:
- Headache
- Shaking
- Sweating
- Nausea or vomiting
- Anxiety and restlessness
- Stomach cramps and diarrhea
- Trouble sleeping or concentrating
- Elevated heart rate and blood pressure
- How to quit alcohol?

As mentioned here, alcohol consumption is the reason behind the risk of erectile dysfunction. Thus, primary treatment involves the inhibition of alcohol consumption which involves various strategies such as:
- Avoid the things that trigger your urge to drink
- Practice saying “no” to alcohol in social situations
- Remind yourself of your reasons for not drinking
- Evaluate the costs and benefits of drinking
- Quit alcohol by diminishing the requirement day by day. Keep a “diary” of your drinking
- Pick a day or two each week when you will not drink at all
- When you’re struggling with alcohol cravings, try strategies such as talking to someone you trust, distracting yourself until the urge passes, accepting the urge and ride it out, instead of trying to fight it, etc.
- Try to have exercise as more as possible and as much scheduled as possible.
- Prescription for erectile dysfunction
 Phosphodiesterase inhibitors (sildenafil, tadalafil, vardenafil and avanafil) improve the relaxation of smooth muscle. Phosphodiesterase inhibitors are also contra-indicated in patients in whom vasodilation or sexual activity are inadvisable, and where there is previous history of non-arteritic anterior ischaemic optic neuropathy, hypotension.
Phosphodiesterase inhibitors (sildenafil, tadalafil, vardenafil and avanafil) improve the relaxation of smooth muscle. Phosphodiesterase inhibitors are also contra-indicated in patients in whom vasodilation or sexual activity are inadvisable, and where there is previous history of non-arteritic anterior ischaemic optic neuropathy, hypotension.
Try herbal remedies which are devoid of side effects. These herbal remedies include ginseng, DHEA (Dehydroepiandrosterone), L-arginine, fenugreek, etc. Any prescription to be taken for erectile dysfunction should be after consultation with doctor because the dose and schedule of medicine depends upon the severity of the disease which can only be interpreted by the doctor specializing in that particular field.

REFERENCES
- http://www.medscape.com/viewarticle/561022
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2917074/
- http://ac.els-cdn.com/S1879522610600371/1-s2.0-S1879522610600371-main.pdf?_tid=7dca7996-f02e-11e6-9bfb-00000aacb35f&acdnat=1486799495_cd2da630bae9a3ad11fb90a2be966fc8
- http://alcoholrehab.com/alcoholism/alcoholism-and-sexual-dysfunction/
- http://www.impotence-guide.com/alcohol-impotence.html
- https://www.helpguide.org/articles/addiction/alcohol-addiction-treatment-and-self-help.htm
- http://patient.info/in/doctor/erectile-dysfunction
- http://www.healthline.com/health/erectile-dysfunction/ed-natural-treatments#Acupuncture9
DIABETIC EYE DISEASE is a serious condition to be found in the diabetic individuals who face problem in their eyes. This disease has the potential to cause severe vision loss and blindness. Diabetic eye disease has no early stage symptoms. There is no pain and vision may not change until the disease becomes severe. It is always shown when the disease starts to spread in the whole eye resulting in blurred vision.
Diabetic eye disease comprises a group of eye conditions including
- Diabetic retinopathy
- Diabetic macular edema (DME)
- Cataract
- Glaucoma
- DIABETIC RETINOPATHY

As its name shows, this eye disease is related to “diabetes” and “retina”. The high blood sugar affects the tiny blood vessels in the light-sensitive tissue called the retina that lines the back of the eyes, causing diabetic retinopathy. It can cause blood vessels in the retina to leak fluid or hemorrhage (bleed), distorting vision. Thus, it is the most common cause of vision loss among people with diabetes.
It is the leading cause of vision impairment and blindness among working-age adults. Because diabetic retinopathy often goes unnoticed until vision loss occurs, people with diabetes should get a comprehensive dilated eye exam at least once a year.
Who is likely to get diabetic retinopathy?
Anyone suffering with diabetes can develop diabetic retinopathy. The longer someone has diabetes, the more likely he or she will get diabetic retinopathy. It is estimated that 40-45% of those with diagnosed diabetes have some degree of diabetic retinopathy.
How is it diagnosed?
Eye examination is done to detect diabetic retinopathy. The eyes should be dilated during the exam, which means eye drops are used to enlarge the pupils. This dilation allows the eye care professional to see more of the inside of the eyes to check for signs of the disease.
- DIABETIC MACULAR EDEMA (DME)

A consequence of diabetic retinopathy, DME is swelling in an area of the retina called the macula. This occurs due to the building-up of fluid called edema in the macula. The macula is very important for the sharp, straight-ahead vision which is important for reading, driving and recognizing faces.
DME is the most common cause of vision loss in individuals with diabetic retinopathy. About half of the people with diabetic retinopathy will develop DME. Although, it is more likely to occur as the diabetic retinopathy worsens, DME can happen at any stage of the disease.
Often, DME is associated with:
- Diabetes for an extended amount of time
- Severe hypertension (high blood pressure)
- Fluid retention
- Hypo-albuminemia (low levels of protein in body fluids)
- Hyperlipidemia (high levels of fats in the blood)
What could be the symptoms for DME?
Common symptoms of DME are blurry vision, floaters, double vision and eventual blindness if it goes untreated.
- CATARACT
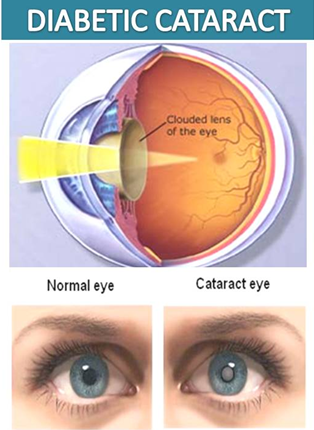
Diabetic Cataract is a condition when the eye’s naturally clear lens becomes cloudy. Adults with diabetes are 2-5 times more likely than those without diabetes to develop cataract. Cataract also tends to develop at an earlier age in people with diabetes.
How diabetes contributes in developing cataract?
Light doesn’t pass through the lens as it should and isn’t properly reflected onto the retina (the light-sensitive tissue lining the back of the eye). As a result, vision becomes cloudy, distorted or blurry.
The eye’s lens gets its nutrients from aqueous humor which is the fluid filling the front portion of the eye. Aqueous humor provides oxygen and glucose as an energy source for the body’s cells. In diabetic condition, sugar levels rise in the aqueous humor and in the lens. High levels of glucose in the lens cause it to swell, affecting clarity of the vision.
The lens also has an enzyme that converts glucose to a substance called sorbitol. When sorbitol collects in the lens, it can affect cells and naturally-occurring proteins, causing the lens to become less clear and more opaque. This condition eventually leads to cataract formation.
- GLAUCOMA
Diabetic Glaucoma is a group of diseases that damage the eye’s optic nerve – the bundle of nerve fibers that connects the eye to the brain. Some types of glaucoma are associated with elevated pressure inside the eye. In adults, diabetes nearly doubles the risk of glaucoma.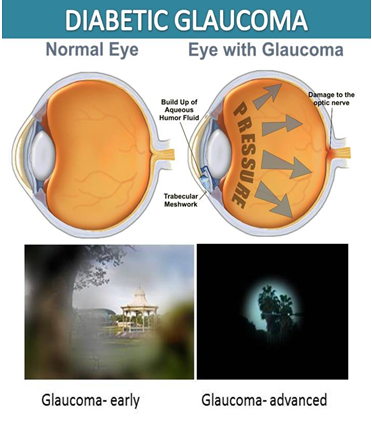
How diabetes contributes in developing glaucoma?
Under diabetic condition (high blood glucose), the retina becomes starved of oxygen and starts to develop new blood vessels & stimulus for these newly developed blood vessels. This triggers new blood vessel formation in the ocular anterior segment and interferes with the normal internal drainage system of the eye leading to elevated intraocular pressure, a condition referred to as glaucoma. If the pressure is high or continues for a long time, usually years, the nerve at the back of the eye may become damaged, and eventually the sight may be affected.
What are the symptoms of this eye problem (glaucoma)?
There may be no symptoms of this eye problem at all until the disease is very advanced and there is significant vision loss. In the less common form of this eye problem, symptoms can include headaches, pain in the eye, blurred vision, watering eyes, halos around lights and loss of vision.
PREVENTION & TREATMENT
- Treatment of diabetes: If you are diabetic, you can help prevent or slow the development of diabetic retinopathy by treating diabetes through:

- Taking the prescribed medication for diabetes
- Sticking to diet
- Exercising regularly
- Controlling high blood pressure
- Avoiding alcohol and smoking
- Treatment of diabetic retinopathy varies depending on the extent of the disease. People with diabetic retinopathy may need laser surgery to seal leaking blood vessels or to inhibit other blood vessels from leaking. Your doctor might need to inject medications into the eye to decrease inflammation or stop the formation of new blood vessels.
People with advanced cases of diabetic retinopathy might need a surgical procedure to remove and replace the gel-like fluid in the back of the eye, called the vitreous. Surgery may also be needed to repair a retinal detachment. This is a separation of the light-receiving lining in the back of the eye.
- Treatment of diabetic macular edema (DME) can be treated with several therapies that may be used alone or in combination. Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Available anti-VEGF drugs include bevacizumab, ranibizumab, and aflibercept which are approved by the U.S. Food and Drug Administration (FDA) for treating DME.
In focal/grid macular laser surgery, a few to hundreds of small laser burns are made to leaking blood vessels in areas of edema near the center of the macula. Laser burns for DME slow the leakage of fluid, reducing swelling in the retina.
Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME. But DME patients who use corticosteroids should be monitored for increased pressure in the eye and glaucoma.
- Treatment of glaucoma requires lowering the eye’s pressure by increasing the drainage of aqueous humor or decreasing the production of the fluid. Medications can accomplish both of these goals. The basic treatment for glaucoma in diabetes is eye drops, and the commonest is one of the beta-blocker drops such as betaxalol, teoptic (cartelol), or timolol.
- Treatment of cataract involves surgery in which the lens is removed and replaced with an artificial one.Cataract surgery is generally safe, so the point at which an operation is undertaken depends partly on the individual.
REFERENCES
- https://nei.nih.gov/diabetes/content/english/faq
- https://en.wikipedia.org/wiki/Macular_edema
- https://nei.nih.gov/health/diabetic/retinopathy
- http://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/basics/definition/con-20023311
- http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy?sso=y
- https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
- https://www.vsp.com/diabetic-macular-edema.html
- https://www.aao.org/eye-health/tips-prevention/diabetes-cataracts
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3589218/
- https://www.hindawi.com/journals/joph/2010/608751/
- https://www.glaucomafoundation.org/news_detail.php?id=194
- http://www.diabeticretinopathy.org.uk/diabetes_glaucoma.html
- http://www.medicinenet.com/diabetes_and_eye_problems/page2.htm



