Nowadays, diabetes, particularly type 2 diabetes, is one of the fastest growing chronic diseases in the society. Tight blood glucose control, dietary requirements and intake of regular medication are only few things that a diabetic patient needs to manage in order to prevent long-term complications. Assured continuity of care does not only create many challenges for the patient but also for the treating physician who will need to support the patient’s management strategies.
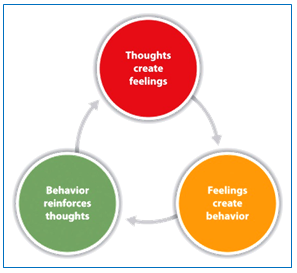
PATIENT EMPOWERMENT refers to a process that enables and facilitates behaviour change. The key to empowerment does not necessarily means better compliance to what the doctor says or prescribes but rather in the opportunity to increase patients’ self-sufficiency to improve their decision-making capabilities.
Research has shown that diabetes education is central to effective self-management behaviour, which in the long term can influence clinical and psychological outcomes.
Approaches have now moved from purely educational interventions to those that empower patients based on the assumption that they are managers of their own health. Diabetes education together with patient empowerment has shown to be the key for effective self-management behaviour. When delivered through information and communication technologies (ICT), this solution has shown to lead to better health outcomes.
KEY ELEMENTS OF EMPOWERMENT

- Diabetes awareness
- Education & training
- Support of healthcare providers
CHARACTERISTICS OF AN EMPOWERED ACTIVATED PATIENT

- He understands his health condition and its effect on his body.
- He feels able to participate in decision-making with his healthcare professionals.
- He actively seeks out, evaluates and makes use of information.
- He feels able to make informed choices about treatment.
- He is able to challenge and ask questions of the healthcare professionals providing their care.
- He takes responsibility for his health and actively seeks care only when necessary.
- He understands the need to make necessary changes to his lifestyle for managing their conditions.
HOW TO EMPOWER PATIENTS?

- DIABETES EDUCATION
Diabetes education for the nurses is vital in forming solid knowledge that will equip them to be able to properly educate their patients.
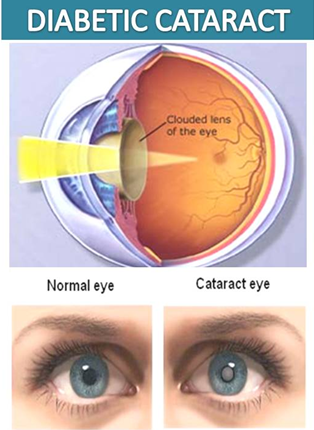
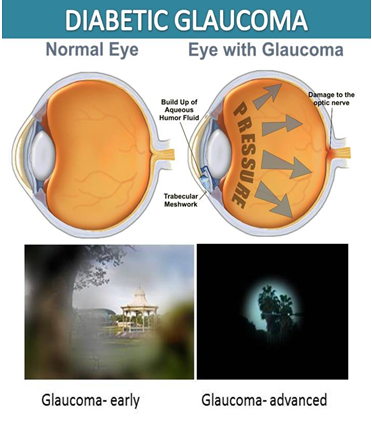
Poor education not only reflects in poor health for the patient but also leads to serious complications and early death imposing a large economic burden on the individual and healthcare systems.
Benefit: This would reduce excess costs for emergency department care and care needed for complications concerning uncontrolled diabetes. A lot of the complications that diabetics face could be prevented easily.
There is a large amount in the community of diabetics that simply do not care about their nutrition or health and are unwilling to make any sort of lifestyle change, those people aside; there is no excuse for the overwhelming amount of complications that some diabetics suffer from due to the lack of knowledge.
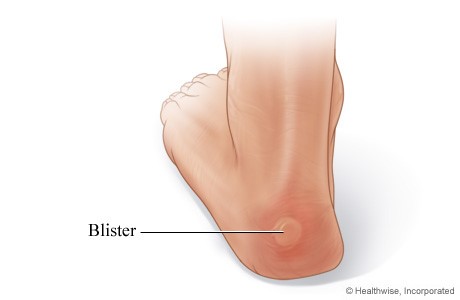
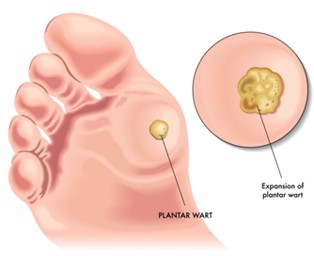
A patient with uncontrolled diabetes deals with physical ailments; people with uncontrolled type 1 diabetes often feel ill, experience cognitive dysfunction, have difficulty maintaining their weight at a desired level, and experience fluctuating moods.
Diabetes education can greatly decrease hypoglycemic events in patients with diabetes.
- SELF MANAGEMENT
 Self-management is seen as a key capability for Patient Empowerment and emphasises that persons with chronic diseases has the central role in managing their health.
Self-management is seen as a key capability for Patient Empowerment and emphasises that persons with chronic diseases has the central role in managing their health.
Self-management is what people do to manage their diabetes or other chronic condition and its effects on their physical health, daily activities, social relationships and emotions.
Mindful eating: Mindful eating empowers the patient to make flexible decisions through the challenges of life. Mindful eating is one way to get closer to meeting the true needs and in the process gradually allows a person to live the life more fully.
Putting someone on a diet that says to avoid rice, “sweets”, “anything white” or “everything fried” automatically creates cravings and (even worse) guilt if they finally respond to their cravings. When a person gives into their cravings, the patient takes the wrong way & fails to manage diabetes.
- INTERNET
 Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.
Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.
The key issue for patients & healthcare professionals is how to deliver personalised behavioural support in ways that are affordable and can reach to maximum number of patients. The internet offers several advantages in this regard because it is available 24 hours a day with very low cost.
Benefits
- It does not require large investments.
- It does not imply high fees.
- It can easily be enriched with new information which immediately becomes available to the target group of users in any location in the world.
- Help patients to monitor their diet and medicinal doses
- Help both the patient and doctor to monitor the long term effect of the interventions
We cannot empower patients!
We only can provide a framework (tools, services, etc.) that makes it easier for patients to empower themselves.
REFERENCES
- http://www.idb.hr/diabetologia/02no1-1.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4372173/
- http://www.reaction-project.eu/downloads/clustering%20event/EMPOWER.pdf
- http://ceur-ws.org/Vol-532/paper11.pdf
- http://www.dnaindia.com/health/report-mindful-eating-empowering-patients-with-diabetes-to-take-charge-of-their-diet-2145200





 Self-management is seen as a key capability for Patient Empowerment and emphasizes that persons with chronic diseases has the central role in managing their health.
Self-management is seen as a key capability for Patient Empowerment and emphasizes that persons with chronic diseases has the central role in managing their health. Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.
Only the internet allows us to set up an independent global diabetological service. The only thing users would need a computer and access to the internet. This service can serve unlimited number of people in the world along with medical consultation.