Menstrual cycle disorders can cause a woman’s periods to be absent or infrequent. Although some women do not mind missing their menstrual period, these changes should always be discussed with a healthcare provider because they can signal underlying medical conditions and potentially have long-term health consequences. A woman who is Suffering from Irregular Periods i.e misses more than three menstrual periods (either consecutively or over the course of a year) should see a healthcare provider.
Amenorrhea – Amenorrhea refers to the absence of menstrual periods, and is classified as either:
● Primary (when menstrual periods have not started by age 15)
● Secondary (when menstrual periods are absent for more than three to six months in a woman who previously had periods)
Oligomenorrhea — Oligomenorrhea is the medical term for infrequent menstrual periods (fewer than six to eight periods per year).
The causes, evaluation, and treatment of amenorrhea and oligomenorrhea are similar and will be discussed together.
CAUSES OF IRREGULAR PERIODS
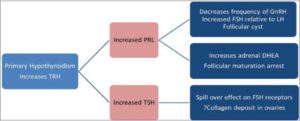
The brain (including the hypothalamus and pituitary gland), ovaries, and uterus normally follow a sequence of events once per month that helps to prepare the body for pregnancy. Two hormones, Follicle Stimulating Hormone (FSH) and Luteinizing hormone (LH), are made by the pituitary gland. Two other hormones, progesterone, and estrogen are made by the ovaries.
Menstrual cycle disorders can result from conditions that affect the hypothalamus, pituitary gland, ovaries, uterus, cervix, or vagina.
Primary amenorrhea — Some of the more common causes of primary amenorrhea include the following:
● Conditions that are present at birth, but may not be noticed until puberty. These conditions include genetic or chromosomal abnormalities and abnormalities of the reproductive organs (e.g, if the uterus is not present or developed abnormally).
● All of the conditions that lead to secondary amenorrhea can also cause primary amenorrhea.
Secondary amenorrhea — Pregnancy is the most common of secondary amenorrhea. Other common causes include the following:
● Ovarian conditions, such as polycystic ovary syndrome and ovarian insufficiency (early menopause).
● Hypothalamic Amenorrhea. This occurs when the hypothalamus slows or stops releasing GnRH (gonadotropin releasing hormone), a hormone that influences when a woman has a menstrual period.
Hypothalamic amenorrhea is associated with low body weight (defined as weighing 10 percent below ideal body weight), a low percentage of body fat, eating disorders such as anorexia nervosa or bulimia nervous, emotional stress, strenuous exercise, and some medical conditions or illnesses. However, in some cases, there is no obvious explanation for hypothalamic amenorrhea.
● Prolactin-secreting pituitary tumors are another common cause of secondary amenorrhea.
Oligomenorrhea — Many of the conditions that cause primary or secondary amenorrhea can also cause a woman to ovulate irregularly). However, most women who develop infrequent periods have polycystic ovary syndrome.
EVALUATION OF IRREGULAR PERIODS
The evaluation of amenorrhea/oligomenorrhea includes a complete medical history and physical examination.
History — There are often clues about the cause of amenorrhea in a woman’s personal and family medical history. A woman should mention if she had any health problems during infancy or childhood, when her first period started (if there was the first period) and how frequently periods have occurred since. If known, the woman should also mention if there is any family history of Suffering from Irregular Periods
Other important points include Suffering from Irregular Periods are the presence of discharge from the breasts, hot flashes, adult acne, facial or chest hair, and headaches or impaired vision. The clinician will also ask about any medications, herbs, and vitamins used, recent stress, recent gynecologic procedures, changes in weight, diet, or exercise patterns, and illnesses.
Physical examination — During the physical examination, the provider will examine the face, neck, breasts, and abdomen. A pelvic examination will also be performed.
Testing — Depending upon the individual, the clinician may order blood tests. Because pregnancy is the most common cause of secondary amenorrhea, a pregnancy test is usually recommended for women whose menstrual periods have stopped. Blood tests to measure hormone levels will also be ordered.
In selected cases, a magnetic resonance imaging (MRI) test may be done to determine if there are hypothalamic or pituitary gland abnormalities in the brain. Occasionally, these causes Suffering from Irregular Periods in women with a suspected chromosomal abnormality, a chromosome analysis may be recommended. A pelvic ultrasound may be recommended to identify abnormalities of the uterus, cervix, and vagina.