Pushing diabetics to take insulin is a medical scam: Fiona Godlee
With diabetes becoming such an epidemic in India, we need to look at the root causes and put money there rather than putting people on insulin.
Category: Fenfuro Blogs
DRUG-INDUCED DIABETES
DIABETES is a well-known disease these days. It occurs when the sugar or glucose levels rise inside the human body. This rise in blood sugar levels takes place due to abnormal functioning of the cells known as β-cells of pancreas.
Under normal conditions, these cells release insulin on requirement to transfer glucose from blood to the tissues/cells for energy. This transfer balances blood sugar levels. The misconduct of these β-cells disturbs the balance of blood sugar levels and causes diabetes.
The activity of β-cells can be disturbed due to many reasons. One of those reasons is the consumption of some therapeutic agents.
THERAPEUTIC AGENTS can influence the development of diabetes, especially when pre-existing risk factors are present and these may cause glucose control to deteriorate if administered to those with existing diabetes.
It has been found that drug-induced diabetes can develop at the age of 20 years but it is more prone at the age between 40-60 years. The chances of development of drug-induced diabetes are found to be more in females (70%) as compared to males (30%).
ACTION OF DRUGS INDUCING DIABETES
Therapeutic agents causing diabetes may act either by increasing insulin resistance or by affecting the secretion of insulin or both.

- Grouping of drugs according to the mechanism of inducing diabetes
- Drugs that cause diabetes by interfering with insulin production & secretion are:
| β-receptor antagonist
(used in hypoglycemia) |
Tacrolimus
(immunosuppressant used in organ transplant) |
| Priminil (Vacor)
(used as rodenticide) |
Didanosine
(used as anti-retroviral therapy) |
| Pentamidine
(antimicrobial medication in used in pneumonia) |
L-asparaginase
(as anti-cancer agent) |
| Diphenylhydantoin
(used as anticonvulsant or antilepptic drug) |
Opiates
(used as pain reliever) |
- Drugs that cause diabetes by developing insulin resistance:
| Glucocorticoids
(to control and treat inflammation) |
β-receptor antagonist
(used in hypoglycemia) |
| Megasterol acetate
(used as anti-cancer drug & appetite stimulant) |
Growth hormone
(growth stimulant) |
| Oral contraceptives
(used to prevent pregnancy) |
Protease inhibitors
(used as anti-retroviral therapy) |
- Drugs that act both on insulin secretion and resistance:
| Thiazide diuretics
(to control blood pressure) |
Diazoxide
(used in treatment of acute hypertension) |
| Cyclosporine
(immunosuppressant used in organ transplant) |
Atypical antipsychotic
(used to treat psychotic conditions) |
- Treatments that induce diabetes by increasing nutrient flux:
| Nicotinic acid
(used in dyslipidemia) |
Total parenteral nutrition
(used in intravenous feeding of person) |
- Grouping of drugs according to the capability of inducing diabetes
These agents may be divided into widely used medications that are weakly diabetogenic and drugs used for special indications that are more strongly diabetogenic.
- Weakly diabetogenic medications include antihypertensive agents, statins and oral contraceptive pills.
- Strongly diabetogenic include steroids, antipsychotics and a range of immunosuppressive agents.
- There are also a number of known β-cell poisons including the insecticide Vacor, alloxan and streptozotocin which can cause permanent diabetes.
TREATMENT & PREVENTION STRATEGIES
- Management of drug-induced diabetes is important as the diabetes so developed can convert into permanent diabetes for whole life. To prevent the development of diabetes, the blood glucose levels should be monitored regularly.
- In cases in which the drug that induced diabetes must be continued, insulin therapy is the most efficacious approach. The diabetics should also try to use the lowest effective dose of therapeutic drug, if possible. Whenever is the possibility, the therapy should be altered.
- A drug which is supposed to have adverse effect on blood glucose level should be avoided in a patient of diabetes, pre-diabetes or insulin resistance.

Other diabetes management strategies include:
- Healthy eating: Lifestyle management is the utmost requirement in the management of drug-induced diabetes. The sweets and fats should be avoided as much as possible. Fruit juice should also be limited. Meals should not be taken more than 3 times a day. Alcohol intake should also be avoided (not more than 1-2 drinks/day) and blood glucose levels should be monitored before & after drinking.
- Exercise: In drug-induced diabetes, physical activity
contributes greatly towards the improvement in health. 30 minutes of moderate activity is recommended on regular basis by physicians. It is also required to check the glucose levels before & after the physical activity. The meal should also be planned according to the blood glucose levels checked previously.
physical activity. The meal should also be planned according to the blood glucose levels checked previously. - Fenugreek supplementation: Another approach to tackle the drug-induced diabetes is by the treatment of diabetes along-with the on-going therapeutic drugs. It has been reported by many researchers that fenugreek is effective in the management of diabetes mellitus. In animal studies, the diabetes was induced in the animals with the help of alloxan or streptozotocin. Then, they were treated with fenugreek supplements. After some days of treatment on animals, improvements were noticed. There was improvement in the blood glucose levels on regular consumption of fenugreek supplements.

In an animal study conducted by Babu KR et al., it was seen that fenugreek extract produced hypoglycemic effect in alloxan-induced diabetic rats after 7-21 days of oral administration. Their histopathological study on the rats showed that the alloxan-damaged β-cells were also restored on treatment with fenugreek extract.
It has been reported by Gaddam A et al. that fenugreek act by controlling the insulin resistance. The hypoglycemic effect of fenugreek was reported by them in their clinical study on both male and female volunteers having diabetes.
In a clinical study conducted by Verma N et al., fenugreek seed extract (Fenfuro™) exhibited anti-diabetic activity in male & female volunteers diagnosed with type 2 diabetes mellitus. On completion of their clinical study, they found reduction in both fasting plasma and post-prandial blood sugar levels in 83% of the study subjects. Fenfuro™ was also safe during & after the study treatment.
According to many reported animal and human studies, fenugreek is safe and effective in the management of diabetes whether induced by drugs or develops itself. Being an herbal supplement, it does not caused any side effect in any animal or human volunteer.
REFERENCES
- https://www.ncbi.nlm.nih.gov/pubmed/1445173
- https://www.patientslikeme.com/conditions/845-medication-induced-diabetes-mellitus
- https://books.google.co.in/books?id=hgiuDHVUuT4C&pg=PA884&lpg=PA884&dq=nicotinic+acid+and+nutrient+flux&source=bl&ots=icmNhQStDJ&sig=dz40cKhJTO_Rvp70CEY8SPxqPSE&hl=en&sa=X&ved=0ahUKEwisy_SQ-5DQAhVBPo8KHczeAmwQ6AEIHzAA#v=onepage&q=nicotinic%20acid%20and%20nutrient%20flux&f=false
- http://www.cancer.med.umich.edu/files/steroid-induced-diabetes.pdf
- http://www.apiindia.org/pdf/medicine_update_2010/diabetology_08.pdf
- http://www.diapedia.org/other-types-of-diabetes-mellitus/41040851133/drug-induced-diabetes
- http://spectrum.diabetesjournals.org/content/24/4/234
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4591578/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2816457/
- http://www.ijddr.in/drug-development/antidiabetic-and-histopathological-analysis-of-fenugreekextract-on-alloxan-induced-diabetic-rats.pdf
- https://www.researchgate.net/publication/309021517_A_multicenter_clinical_study_to_determine_the_efficacy_of_a_novel_fenugreek_seed_Trigonella_foenum-graecum_extract_Fenfuro_in_patients_with_type_2_diabetes
Hypertension & Diabetes
Blood pressure is the force of blood against your blood vessels as it circulates. This force is necessary to make the blood flow, delivering nutrients and oxygen throughout your body. High blood pressure, also called hypertension, means there is too much pressure in your blood vessels. It may precede the onset of diabetes mellitus (DM). In many of the cases, both hypertension and diabetes mellitus may be diagnosed together. Diabetic population has almost doubled occurrence of hypertension as compared to non-diabetic general population.
Diabetes and high blood pressure are considered as major cardiovascular risk factors, which mean these can lead to coronary artery disease, stroke, left ventricular hypertrophy, and nephropathy. Patients suffering from both diabetes and high blood pressure have greater risk of atherosclerosis.
What are causes of high blood pressure?
Are you diagnosed with blood pressure & diabetes?
If yes, then monitor yourself regularly
Learn how to measure blood pressure & blood sugar at home, keep record of these.
What are the recommendations for starting anti-hypertensives?
British Hypertension Society, British Hyperlipidaemia Association and British Cardiac Society have jointly suggested the initiations of treatment of hypertension in diabetics when BP is equal to or more than 140/90 mm Hg. According to the WHO Expert Committee Recommendation in Hypertension Control treatment may be instituted at BP 130/85 mm Hg in a patient with diabetic nephropathy
Are lifestyle modifications recommended for Diabetic hypertensives?
Lifestyle modifications are must for diabetic hypertensive patients. These modifications also correct obesity, hyperglycaemia, hyperinsulinaemia, and act as primary prevention against cardiovascular risks. These will reduce blood pressure and control blood glucose levels.
It has been observed that regular physical activity has an independent cardioprotective effect. Regular aerobic exercise can reduce systolic BP by an average of 4 mmHg and diastolic BP by an average of 2.5 mmHg. It is advised to all patients to become physically active, as part of a comprehensive plan to control hypertension and diabetes, regardless of drug treatment. Aim for 30 minutes of moderate-intensity physical activity on most, if not all, days of the week.
Quitting smoking
Quitting smoking may not directly reduce BP, but markedly reduces overall cardiovascular risk. The risk of myocardial infarction is 2–6 times higher and the risk of stroke is 3 times higher in people who smoke than in non-smokers.
Quitting smoking also helps in better management of blood glucose and HbA1c levels.
Dietary Modification
Adequate intake of dietary-fibre, and K+, Ca++, Mg++ from fresh fruit, green vegetables, and dairy products should be ensured. Mg++ is provided by chlorophyll of green leafy vegetables. Anti-obesity diet should not contain more than 1/3rd of total calories from fat. Of the fat calories, 1/3rd should be derived from saturated fat and 2/3 from poly- or monounsaturated fat.

Weight reduction
Every 1% reduction in body weight lowers systolic BP by an average of 1 mmHg. Weight reduction by as little as 4.5 kg reduces BP and/or prevents hypertension in a large proportion of overweight people. Weight loss of 10 kg can reduce systolic BP by 6–10 mmHg.

Reducing Alcohol Intake
Reducing alcohol intake may reduce BP in many patients and also contributes in better management of blood sugar levels.
Co-existence of diabetes mellitus and hypertension increases the risk of macro – and micro-vascular complications. Blood pressure should be measured in supine, sitting, and standing postures in a diabetic patient to detect existence of autonomic neuropathy and drug induced postural hypotension. A good BP control (130/80 or below) prevents or retards the progress of both micro and macro-vascular complications. Tight control of blood glucose levels prevents or delays the progress of micro-vascular complications.
It is very important and must of diabetic hypertensive patients to modify their lifestyle to lead a healthy and happy life.
FenfuroTM is a clinically evaluated dietary supplement for effective management of blood glucose levels. It is supported by 6 international patents.

References
- http://www.webmd.com/hypertension-high-blood-pressure/guide/hypertension-treatment-overview#1
- http://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/high-blood-pressure/art-20046974
- http://care.diabetesjournals.org/content/26/suppl_1/s80
- http://www.healthline.com/health/type-2-diabetes/hypertension#Overview1
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3314178/
INSULIN: HEALTH RISKS
Insulin hormone is a chemical messenger secreted by the beta cells of pancreas, which allows the body to utilize glucose from carbohydrates and convert the extra glucose into energy for future use. Insulin maintains the sugar balance in the body by keeping blood sugar level from getting too high (hyperglycemia) or too low (hypoglycemia). Glucose obtained from the food does not directly convert into energy. When we eat food, the blood sugar levels rise and beta cells of the pancreas are then signaled to release insulin into the blood stream. Then the released insulin absorbs the sugar by binding to insulin receptors and converts excess of the sugar in glycogen (energy), which get stored in the liver. It has dual mode of action i.e. an excitatory one and an inhibitory one:
- It stimulates glucose uptake and lipid synthesis.
- It inhibits the breakdown of lipids, proteins and glycogen, and inhibits the glucose pathway (gluconeogenesis) and production of ketone bodies (ketogenesis).
Sometimes glucose metabolism gets impaired, characterized by hyperglycemia which may be due to either pancreas does not secrete insulin or insulin receptors do not respond to the insulin properly. This condition is also known as diabetes mellitus. So it becomes essential to take the insulin externally.

Endogenous insulin (that which is found naturally in the body) acts on the principle of feedback. If glucose levels rise when eating something sweet, insulin secretion is increasing, too.
Exogenous insulin Patients suffering from Type I Diabetes are treated by doses of insulin produced by sources external to the body of the patient and administered in addition to the endogenous insulin. This type of insulin produced by sources other than human body is called exogenous insulin.
RISKS OF INSULIN INTAKE
When the insulin metabolism in the body gets impaired, then sometimes it becomes necessary to provide it externally. But there are certain side effects of insulin therapy. These are:
Hypoglycemia: It is the most serious problem associated with insulin therapy and it is also called as insulin reaction. It occurs 
when blood sugar levels fall below the normal limits. If the insulin dose is high, then the blood glucose levels may decrease abruptly and if remain untreated may lead to seizure, death or coma. Hypoglycemia is associated with increased plasma dopamine, epinephrine and plasma renin activity. Signs and symptoms of low blood sugar are feeling weak, drowsy, or dizzy, experiencing shakiness, confusion, anxiety, nausea, or headache, blurred vision and loss of consciousness.
Weight gain
Weight gain during insulin therapy is the common problem that may be presented as edema. Weight gain may be associated with abrupt restoration of glucose control in a patient whose control was poor previously. It may be due to more efficient use of calories during insulin therapy, suggesting additional benefits of dietary and exercise modifications. Insulin therapy leads to increase in body fat as a result of the elimination of glycosuria and reduction in 24-hour energy expenditure which results in an insulin-associated decrease in triglyceride or free fatty acid cycling, glucose and protein metabolism and hence weight gain.

Renal problems
Insulin therapy may also cause renal complications such as decreased renal plasma flow, glomerular filtration rate and significantly increased urinary albumin excretion rate. However, these changes are reversible upon resolution of hypoglycemia. Therefore changes in kidney function during insulin-induced hypoglycemia may result from direct stimulation of the efferent sympathetic nerves to the kidney and hormonal counter regulatory mechanisms.
Allergic reactions
Patients on insulin therapy may experience allergic reactions in response to insulin. Sometimes these reactions may be minor like hives or itchiness, but sometimes may be life threatening such as swollen tongue, tightness in chest, difficulty breathing, dizziness or fainting and may need hospitalization. These reactions may be localized (such as rashes at the injection site) or systemic (itching, redness, muscle cramps.).
Hypophosphatemia
Hypophosphatemia is one of the major metabolic complications of insulin therapy, particularly in the patients who are on treatment of diabetic ketoacidosis (DKA) as insulin increases intracellular phosphate transport. Sometimes hypokalemia and hypomagnesaemia may also occur during insulin therapy.
Skin related complications
Other adverse effects of insulin include loss or overgrowth of fat tissue at injection sites. Repeated use of the same injection site increases the risk of lipoatrophy — with time, patients learn that these areas are relatively pain free and continue to use them. However, the absorption of insulin from lipoatrophic areas is erratic leading to frequent difficulties in achieving ideal blood glucose control.
Lipohypertrophy is the most common cutaneous complication of insulin therapy.
Drug interactions
Exogenous insulin interactions include alpha and beta-blockers and other high blood pressure drugs, steroids, hormone-based contraceptive pills, asthma and cold medications, aspirin, thyroid medications, and even other diabetes drugs.
Administration of exogenous insulin provides a different insulin gradient than that occurring after endogenous insulin secretion. Endogenous insulin secretion acts initially on the liver where a major portion of it is taken up and <50% reaches the peripheral tissues. Exogenously administered insulin must circulate through the peripheral tissues before it can reach the liver; therefore, peripheral hyperinsulinemia is necessary to attain adequate insulin to regulate the liver. Another downside of insulin therapy is the need to increase the dose and the regimen complexity with time, the increase in severe hypoglycemia, and the potential increase in mortality as well as the potential increased risk for specific cancers.
It becomes all the more important for medical practitioner, patients and other stake holders to USE EXOGENOUS INSULIN INTELLIGENTLY, CAUTIOUSLY & JUDICIOULY.
References
- http://www.medicinenet.com/insulin_for_diabetes_treatment_types_side_effects/page2.htm#what_insulin_preparations_are_available
- http://www.endocrineweb.com/conditions/type-1-diabetes/what-insulin
- http://www.medicalnewstoday.com/info/diabetes/whatisinsulin.php
- http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/insulin-basics.html?referrer=https://www.google.co.in/?referrer=http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/insulin/insulin-basics.html
- https://medlineplus.gov/druginfo/meds/a682611.html
- https://www.drugs.com/sfx/insulin-side-effects.html
- http://www.diabeticlifestyle.com/blood-glucose/insulin-side-effects
http://www.iddt.org/about/gm-vs-animal-insulin/allergic-reactions-to-insulin
GLYCAEMIC INDEX is the ranking system of carbohydrate-containing food products including vegetables, grains, fruits, etc. These ranks are calculated in comparison to the reference food i.e. either glucose or white bread. Thus, glycaemic index measures the impact of food products on blood glucose levels.
Glycaemic index falls under the categories of low, medium or high. High glycaemic index diet raises more blood sugar levels as compared to medium or low glycaemic index diet.
 IMPORTANCE OF GI
IMPORTANCE OF GI
After consumption of food, carbohydrates that break down more quickly during digestion and release glucose rapidly into the blood stream tend to have high glycaemic index. Similarly, carbohydrates that break down more slowly, releasing glucose more gradually into the bloodstream tend to have a low glycaemic index. Due to slow release of glucose into blood stream, low-glycaemic index foods tend to prevent diabetes.
Thus, glycaemic index is an important parameter for management of many metabolic disorders. It has been reported that low-glycaemic index diets are associated with decreased risk of cardiovascular disease, type 2 diabetes, stroke, depression, kidney disease, cancers, etc.
GLYCAEMIC INDEX AND DIABETES MEAL
For most of the people with diabetes, first tool for management of blood glucose levels is carbohydrate counting. Glycaemic index is such a tool, which could contribute well to a diabetic person meal for managing type 2 diabetes.
Low glycaemic index diet (GI ≤ 55) will prevent the immediate hike in the blood sugar levels after eating.
 The diet from high GI to low GI can be changed by:
The diet from high GI to low GI can be changed by:
- Including one low GI food at each meal (given in table).
- Choosing breakfast cereals based on barley, oats (such as porridge), and wheat and rice bran.
- Eating grainy breads made with whole seeds, barley and oats instead of white or brown bread.
- Eating pulses and legumes (such as beans, lentils and peas).
- Eating high fiber foods because it helps slow the digestion and absorption of carbohydrates.
BENEFITS OF LOW GLYCAEMIC INDEX DIET IN TYPE 2 DIABETES
- Blood glucose levels are maintained within acceptable range by monitoring the quantity & quality of carbohydrates consumed.
- HbA1c levels are also lowered and come under normal range with intake of low glycaemic index diet.
- Low glycaemic index diet also normalizes the insulin production in diabetic body.
- Low glycaemic index diet also helps to manage LDL cholesterol levels along with free fatty acids. Thus, it is helpful in managing lipid levels.
LOW GI FOODS (GI ≤ 55)
Foods with low GI have been given as following:
| Breakfast cereal | |||
| Bran | 30 | Rolled oats | 51 |
| Oat bran | 50 | Special K | 54 |
| Vegetables | |||
| Frozen green peas | 39 | Tomato | 15 |
| Frozen sweet corn | 47 | Chilies | 10 |
| Raw carrot | 16 | Lettuce | 10 |
| Boiled carrot | 41 | Green beans | 15 |
| Broccoli | 10 | Red pepper | 10 |
| Cauliflower | 15 | Onion | 10 |
| Cabbage | 10 | Mushroom | 10 |
| Bread | |||
| Soya and linseed | 36 | Whole wheat | 49 |
| Wholegrain pumpernickel | 46 | Sourdough rye | 48 |
| Heavy mixed grain | 45 | Sourdough | 54 |
| Fruits | |||
| Cherries | 22 | Plums | 24 |
| Grape | 25 | Peaches | 28 |
| Apples | 34 | Pears | 41 |
| Dried apricots | 32 | Grapes | 43 |
| Coconut | 45 | Coconut milk | 41 |
| Kiwi | 47 | Orange | 40 |
| Strawberry | 40 | Prunes | 29 |
| Legumes | |||
| Kidney beans | 52 | Butter beans | 36 |
| Chick peas | 42 | Red lentils | 21 |
| Green lentils | 30 | Pinto beans | 45 |
| Blackeyed beans | 50 | Yellow split peas | 32 |
| Dairy | |||
| Whole milk | 31 | Skimmed milk | 32 |
| Chocolate milk | 42 | Sweetened yoghurt | 33 |
| Custard | 35 | Soy milk | 44 |
| Snacks & sweet foods | |||
| Nut & seeds bar | 45 | Sponge cake | 46 |
| Nutella | 33 | Milk chocolate | 42 |
| Peanuts | 13 | Walnuts | 15 |
| Cashew nuts | 25 | Nuts & raisins | 21 |
| Jam | 51 | Corn chips | 42 |
| Oatmeal crackers | 55 | ||
| Staples | |||
| Wheat pasta | 54 | Potatoes | 54 |
| Meat ravioli | 39 | Spaghetti | 32 |
| Tortellini | 50 | Egg fettuccini | 32 |
| Brown rice | 50 | Buckwheat | 51 |
| Barley | 22 | Yam | 35 |
| Sweet potatoes | 48 | Noodles | 47 |
TIPS FOR DIABETICS
- Manipulating the sequence in nutrient intake: The glycaemic control in diabetics can be achieved by sequential intake of nutrients. Lipid and protein ingested before carbohydrate reduce postprandial hyperglycemia.Manipulating the sequence of nutrient ingestion might reveal a rapid, feasible, economic and safe strategy for optimizing glucose control in Type 2 Diabetes.
Trico D et al. suggested that high-carbohydrate containing foods should only be consumed after non-glucidic nutrients to combine the positive effects of lipids and proteins on glucose. This manipulation in diet gave a strategy for long-term management of type-2 diabetes.
- Eat unprocessed food: Unprocessed food should be eaten as much as possible. Whole, unprocessed food usually (but not always) has a lower glycaemic index than the same food when it’s processed.

-
Avoid overcooked food: Food should not be overcooked because it raises its glycaemic index.

-
High fiber food: Most of the food that is high in fiber takes longer to digest and raises blood sugar slowly.

CONCLUSION
Considering the impact of carbohydrates on blood glucose levels, glycaemic index improves the chances of picking the best carbohydrates for managing diabetes. Thus, glycaemic index is a useful approach for a diabetic person.
Glycaemic index also helps to maintain the balance between proteins and lipids. This balance manages the blood glucose levels by slowing the process of digestion.
Glycaemic index helps to interpret that which carbohydrate is beneficial for diabetics and which fast food worsens the condition of diabetes. Thus, if you have diabetes, glycaemic index is made for you. Learning a new way to eat takes time and effort but it contributes greatly to manage diabetes.
REFERENCES
- http://www.diabetes.org/
- http://www.whfoods.com/genpage.php?tname=faq&dbid=32
- http://www.diabetes.org.nz/food_and_nutrition/glycaemic_index
- http://www.diabetes.co.uk/diet/glycaemic-index-diet-and-diabetes.html
- file:///C:/Documents%20and%20Settings/Sys1/Desktop/The%20GI%20Diet%20-%20List%20of%20low%20GI%20foods.html
- http://www.healthlinkbc.ca/healthtopics/content.asp?hwid=aba5112
- http://www.nature.com/nutd/journal/v6/n8/full/nutd201633a.html
- http://www.diabetesselfmanagement.com/blog/my-battle-with-the-glycemic-index/

DIABETES MELLITUS
- Diabetes mellitus or diabetes is a condition when there is rise in blood sugar levels in the body. The body becomes unable to use blood sugar (via insulin) for energy. During type 1 diabetes mellitus, pancreas becomes unable to produce insulin due to which glucose remains in the blood instead of transferring to the cells of the body. During type 2 diabetes mellitus, either the pancreas does not produce sufficient amount of insulin or the cells become unresponsive to insulin. In both of the conditions, sugar is not transferred from blood to the cells of the body. Thus, blood sugar levels raise causing diabetes.
(http://www.diabetes.org/diabetes-basics/common-terms/)

- Epidemiology: India has the largest number of diabetic people. According to WHO, there were 32 million people diagnosed with diabetes in year 2000. It is now estimated that they will rise to 80 million by the year 2030. Thus, there is a critical need for the strategies to prevent the epidemic of diabetes.

- Goals for management of diabetes: The goals for managing diabetes in people are to provide:
- Relief from diabetic symptoms
- Prevention of complications such as retinopathy, neuropathy, cardiovascular disease, cerebro-vascular disease, etc
- Prevention of infections
- The primary prevention criteria for diabetes by any healthcare provider include healthy life style focusing on proper balanced diet, increased physical activity and weight control. Lifestyle modification is the cornerstone for the management of diabetes.
- For management of diabetes, dietary modifications are required. They aim to achieve and maintain ideal body weight, euglycaemia and desirable lipid profile.
(http://icmr.nic.in/guidelines_diabetes/guide_diabetes.htm)
(http://icmr.nic.in/guidelines_diabetes/section6.pdf)
ROLE OF DIETARY FIBER
- Dietary fiber: Dietary fiber is the part of plant food, which cannot be digested by human body. Other food components such as fats, proteins & carbohydrates are broken down and absorbed by the human body. But dietary fiber passes intact through the stomach, small intestine, and colon and out of the body.
- Availability: Dietary fiber is mainly found in the fruits, vegetables, whole grains and legumes. It provides health benefits such as maintaining blood sugar levels, healthy weight and preventing heart disease.
- Benefits: The high-fiber diet has many benefits such as,
- Controlling blood sugar levels by slowing the absorption of sugar
- Achieving healthy weight by lowering blood cholesterol levels
- Helps to maintain bowel health
- Decreases chances of constipation
(http://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983)
- Diabetes & dietary fiber
- Dietary fiber is reported to lower blood glucose levels. The daily intake of soluble fiber results in the prevention of diabetes.
- Mechanism: Soluble fiber help to control blood sugar levels by delaying gastric emptying, holding back the entry of glucose into the bloodstream and lessening the postprandial (post-meal) rise in blood sugar. Because fiber slows the digestion of foods, it helps to inhibit the sudden spike in blood glucose that may occur after a low-fiber meal. Such blood sugar peaks stimulate the pancreas to pump out more insulin. The cholesterol-lowering effect of soluble fiber may also help people with diabetes by reducing heart disease risks.

- It has also been proved by the clinical studies that high fiber diet is beneficial to improve glycaemic control, glycosylated hemoglobin and hyperinsulinemia. It has been shown in the study that increases in bile-acid excretion due to dietary fiber intake is responsible for lowering blood glucose levels. The high fiber diet also helped to lower plasma lipid concentrations.
(http://www.nejm.org/doi/full/10.1056/NEJM200005113421903#t=articleTop)
- Epidemiological studies suggested 29% reduction in the development of diabetes due to the protective effect of high dietary fiber intake. Increase in dietary fiber intake resulted in subsequent improvements in glycaemic control, reduction in the use of oral medication and insulin doses. Thus, dietary fiber consumption without altering the energy intake from carbohydrates, proteins and fats reduces the need for medication in type 1 and type 2 diabetic patients.
- Fiber-rich diet for diabetics: It is recommended that an adult male need 38g per day of fiber and female need 25g per day of fiber intake to prevent diseased state. Diabetic individuals should follow following high fiber diet to lower blood glucose levels:
- Skins and seeds of vegetables and fruit
- Whole grain bread, pasta, cereal, crackers and rice
- Barley, beans and lentils
- Canned beans, chickpeas in salads
- Ground flax seeds to yogurt, cereal
- Almonds
- Fenugreek seeds
(http://www.diabetes.ca/diabetes-and-you/healthy-living-resources/diet-nutrition/fibre)
(http://www.webmd.com/diet/guide/fiber-how-much-do-you-need#1)
- Fenugreek as dietary fiber: Fenugreek seeds are reported to be a rich source of dietary fiber. Gel fiber present in fenugreek seeds contribute towards anti-diabetic property. The fiber content of fenugreek helps to lower blood glucose levels and delay gastric emptying, thereby preventing the rise in blood sugar levels. Fenugreek seeds contain 50.2% fiber which have hypoglycemic and hypolipidemic effect in diabetic patients.
- In an animal study, fenugreek seeds extract was administered to diabetic rats. Fenugreek seeds significantly reduced serum cholesterol levels in rats. It was very effective to reduce blood sugar levels also.
- It is reported that consumption of 25g of fenugreek seeds per day exhibit hypoglycemic effect in diabetic patients.
- Thus, dietary modification with fiber will be helpful to reduce blood sugar levels in diabetic patients.
(http://diabeticbar.com/fenufibers.htm)
(http://fenufibre.com/whatIsFenufibre.html)
FenfuroTM is a patented and clinically evaluated product for safe and effective management of blood sugar levels. Fenfuro is a first of its kind, safenutraceutical derived from fenugreek seeds through a patented process. Through its unique scientific process, FENFURO concentrates the bioactive part of plants into a manageable dose, while removing the inert parts such as cellulose. Also, since a lot of healthy botanicals are not palatable, consuming their concentrate in capsule form in small dosage is a lot easier. FENFURO contains a rich variety of saponins and flavonoids. These substances are known to lower blood lipid level and help in insulin sensitization and glucose regulation. FENFURO is the first dual action insulin sensitizer.
A clinical evaluation of FENFURO was carried out on a total of 154 Type 2 diabetics for a period of 3 months, to determine its efficacy and safety. At the end of three months 83% of the patients reported decrease in fasting sugar levels and 89% patients reported decrease in PP sugar levels. The patients also showed significant decrease in HbA1C levels as compared to respective baseline value. 48.8% of patients reported reduction in dosage of anti-diabetic therapy after regularly taking FENFURO.
The statement and product have not been evaluated by the FDA to diagnose, treat, cure or prevent any disease.
DEALING WITH DIABETIC FOOT

DIABETIC FOOT
- Any ulcer or infection developed on foot during diabetic condition is termed as diabetic foot. It is one of the long-term complications of diabetes mellitus (rise in blood sugar levels). Ulcers or wounds most commonly occur at the bottom of the toe of the patient.
- Reasons: Diabetes from very long time causes the damage in the nerves & blood vessels of the body which are the major reason behind diabetic foot.

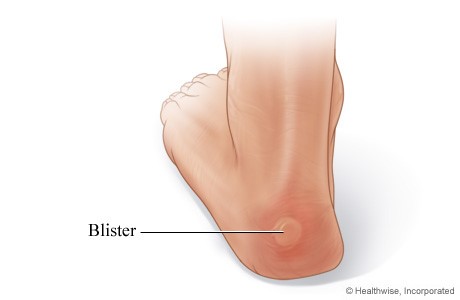
- Nerve damage causes the person to lose feeling in the feet. Due to the loss of feeling, foot is exposed repeatedly to
trauma or injury. Thus, any cut, blister or sore remains undiscovered. So, these minor foot injuries become ulcers & lead to major infections. - Blood vessel damage causes narrowing of the area to flow blood and oxygen throughout feet. Poor circulation of blood and oxygen in the foot area causes the wound healing process to slow down. This further worsens the condition of diabetic foot.
- Sometimes, long-term diabetes loses normal foot arc in the patients. This causes clawed toes or hammer toes, displacement of fat cushion or foot-bottom deformity which further causes abnormal weight bearing in the foot. This changes the shape of the foot. The normal footwear becomes unable to fit properly and pushes the foot towards injury.

- Nerve damage causes the person to lose feeling in the feet. Due to the loss of feeling, foot is exposed repeatedly to
- People with diabetes can develop many foot problems. Neglecting these problems can cause serious conditions which lead to amputation (removal of limb by surgery).
- According to the research data, foot ulcers within diabetic individuals are around 15% and become as high as 25%.
(http://www.diabetes.org/living-with-diabetes/complications/foot-complications/?loc=lwd-slabnav)
(https://medlineplus.gov/diabeticfoot.html)
PREVENTION & TREATMENT OF DIABETIC FOOT
- The primary criteria for prevention and treatment of diabetic foot include the self-management. Foot care is the prime option for diabetic individuals to avoid the foot injury and minimize the chances of the development of diabetic foot.
- Self-care activities: To keep the feet healthy in diabetic individuals, following self-care activities are recommended by healthcare personnel:

- Check your feet everyday for cuts, sores or blisters. You can also use mirror, if necessary.
- Wash your feet everyday in warm and clean water without soaking for long time. Keep your feet dry after washing and be sure to dry your feet between toes.

- Keep the feet soft and smooth. Use cream or lotion to keep them soft after washing. Never use any cream or lotion in-between the toes and fingers because this will lead to infection.

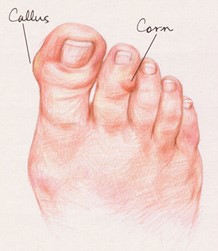
- Corns and calluses should not be cut. Keep them smooth by rubbing gently in one direction.
- Trim the toenails according to the requirement. In case of ingrown toenail, consult doctor. Smooth the nails after trimming. There should not be any toenail left sharp which could cause injury.

- Wear shoes & socks all the time. Do not walk barefoot, not even indoors because it may cause minor injury to the feet. Wear those shoes which fit comfortably in your feet.

- Protect the feet from extreme heat and cold. Put sunscreen lotion on the feet to prevent sunburn. Wear socks whenever you feel cold. Keep the feet away from open fires.
- Physical activities which are easy on the feet should be chosen. Avoid running & jumping. Wear athletic shoes for exercise that fit well and provide good support.
- Try to perform activities which will keep the blood flowing in the feet such as put the feet up while sitting, wiggle the toes after intervals, move the ankles up & down and do not cross legs for longer periods of time.
- Avoid smoking because it can narrow and harden the blood vessels, thus, causes blood vessel damage.
- Check your blood sugar levels regularly.
(http://www.healthsanaz.com/diabetic-foot-care-posters-df19.html)
(https://www.niddk.nih.gov/health-information/diabetes/preventing-diabetes-problems/keep-feet-healthy)
DIABETIC FOOT ASSESSMENT QUESTIONNAIRE
The problems given in the following questionnaire in a diabetic individual should be minutely handled because they can lead to diabetic foot:
- Is there any appearance of corn or calluses?
- Is there any formation of blister on any part of the foot?
- Are there any ingrown toenails?

- Is there any formation of bunion beside the toe?

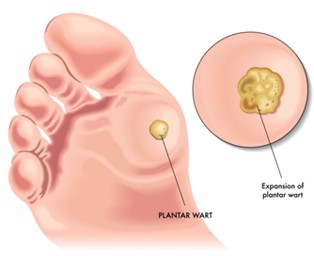
- Is there any appearance of plantar wart at the bottom of the feet?
- Is there any formation of hammer toe?

- Is there any formation of dry and cracked feet skin in grey or red color?

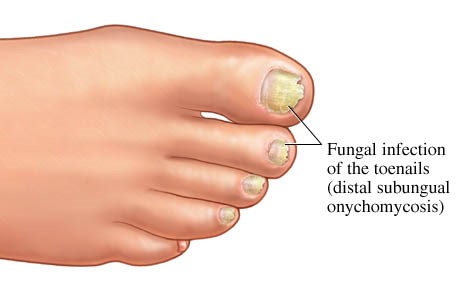
- Is there any appearance of foot toe fungal infection?
- Is there any mild or severe pain in the feet?

“Call or see your doctor right away if you have any of these signs to avoid diabetic foot”



