Some foods, like those with lots of sugar, can cause inflammation. And inflammation can impact the health of your feet.
When most people think about nutrition and their health, they have no trouble associating the foods they eat with weight loss or heart health, says Sherri Greene, DPM, a podiatrist in New York City who practices holistic foot care. However, your diet affects many other parts of your body, including your feet.
“When I explain to people that your feet are connected to the rest of your body, and what you put into your body is what makes up your body, they’re like, ‘Wow!’ When they feel better after they change their diet, then they get it,” she says.
Feet and Nutrition: Fighting Off Inflammation and Pain
One problem linked to nutrition that can affect your feet is inflammation, Dr. Greene says. Certain foods can increase chemicals in your body that cause tissue inflammation. This inflammation could appear in your foot as plantar fasciitis, which causes pain in the thick band of tissue that runs across the bottom of your foot, in your heel, or elsewhere in your foot.
Many common foods in the American diet encourage inflammation, such as the refined grains, sugar, and trans fats in many baked goods and junk foods; the saturated fat in red meat; and the omega-6 fats found in many commonly used vegetable oils, such as corn, soybean, and sunflower oils.
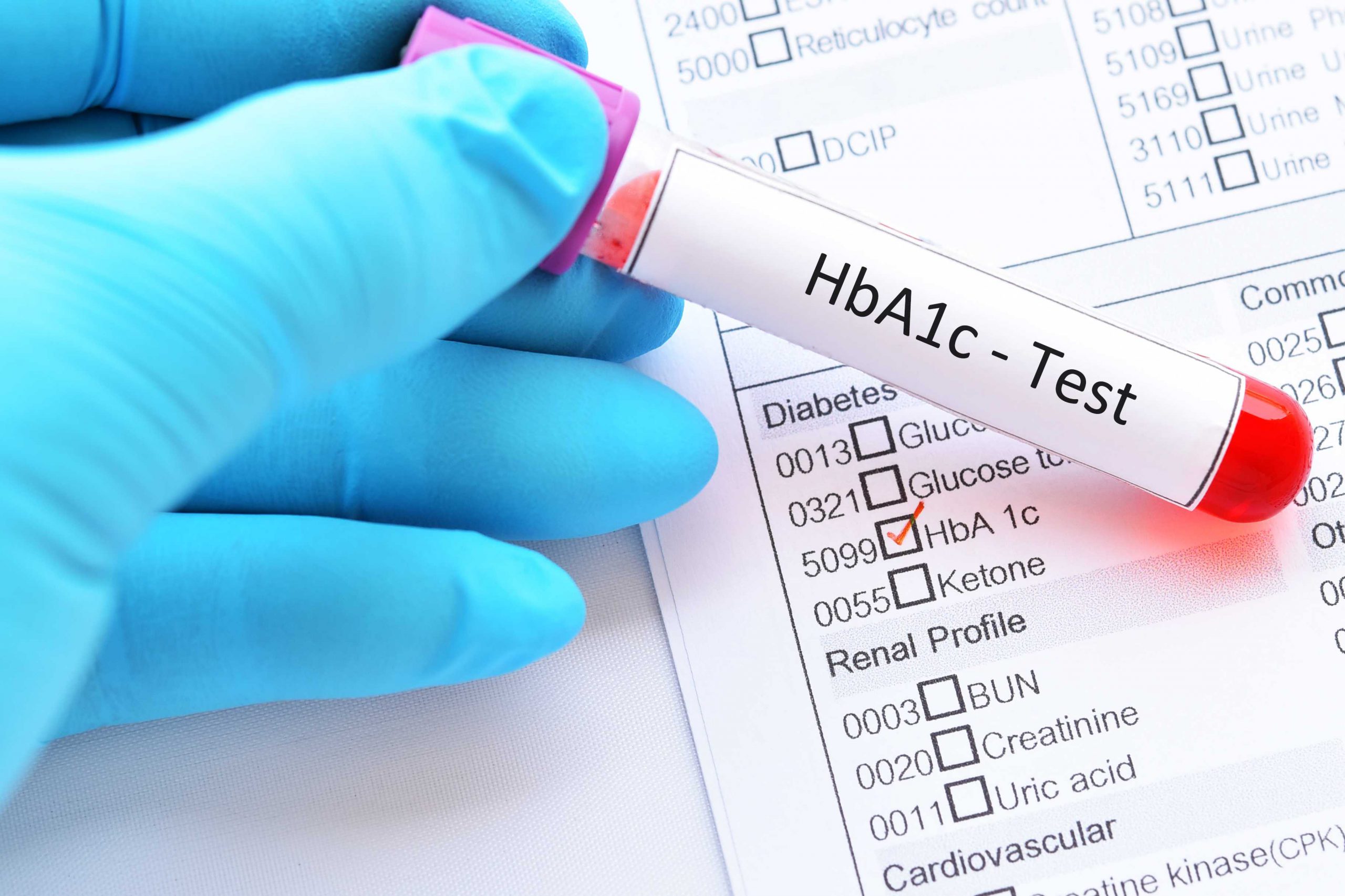
In addition, some people may have increased levels of inflammation in their bodies due to chronic allergies to common foods such as wheat, Greene says. Another factor that can contribute to inflammation is eating too many foods that cause your blood sugar to rise quickly, such as sweets, white flour, and pasta
.
As a result, the nutritional approaches Greene discusses with patients to reduce inflammation include:
Eating more omega-3 fats. Fatty fish such as salmon, as well as fish oil supplements, are good sources of omega-3s, Greene says. Omega-3s help reduce inflammation, and nutrition studies suggest they should be properly balanced in the diet with omega-6s. Most people’s diets provide far more omega-6s than omega-3s, and a fish-rich diet can address this imbalance.
Doing a general diet makeover. Following an overall healthier diet can provide anti-inflammatory benefits to your feet and your total health. This includes eating more green vegetables and other fresh plant foods, and cutting out refined grain foods and sugary treats, Greene says.
Feet and Nutrition: Other Health Connections
Two common conditions that affect millions of Americans’ feet are peripheral artery disease and diabetes. Each of these conditions can harm your feet by damaging arteries that bring blood to your lower extremities.
Good nutrition can also help protect your feet from these conditions. According to the National Institutes of Health (NIH), a diet low in saturated fat, trans fat, and sodium and rich in fruits and vegetables can help reduce your risk of peripheral artery disease. A 2008 study in the Journal of Vascular Surgeryspecifically found that omega-3s were associated with a lower risk of peripheral artery disease.
If you have diabetes, a healthy diet can help protect your feet from complications of that condition, too. In general, the NIH recommends a diet rich in whole grains, beans, vegetables and fruits, lean meats, and a limited amount of fats and sweets for people with diabetes.
Whether you eat more healthfully to counteract a medical condition or to avoid one, following the NIH’s recommendations will help ensure that your feet, along with the rest of your body, continue to serve you well.