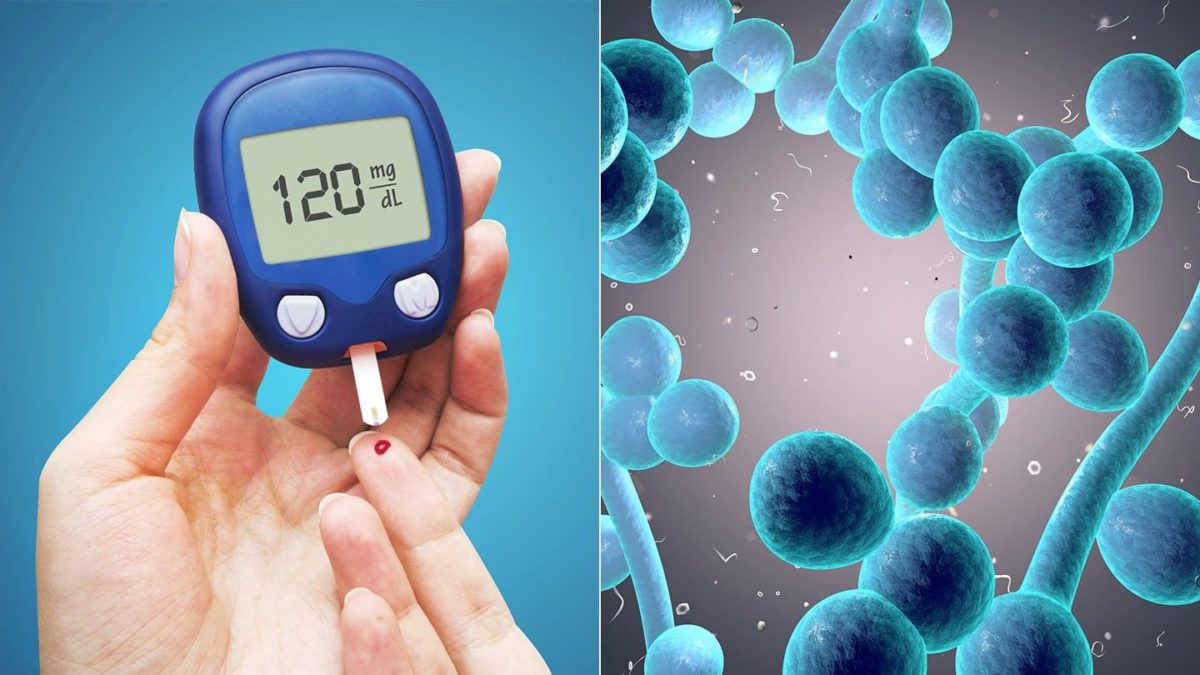
Women with type-2 diabetes are at increased risk of yeast infections because they have more sugar in thier body.
Vaginal yeast infection, also known as candidiasis, is an irritating condition that causes itching and irritation around the vagina, a thick white discharge that looks like cottage cheese, and burning when using the bathroom or having sex. Although many women experience yeast infections, women with type 2 diabetes have them more often.
Type 2 Diabetes: Blood Sugar and Yeast Infections
Most women have yeast organisms as part of their normal flora, the tiny microorganisms that live on and inside our bodies. These microorganisms don’t cause any discomfort or symptoms because they are limited in number. However, when there is overgrowth of these normal organisms, their presence becomes a problem.
“No one knows exactly why yeast infections are more common [in women with type 2 diabetes] but there is a definite association with how well a person’s diabetes is controlled,” says Vincent Woo, MD, chair of the clinical and scientific section of the Canadian Diabetes Association. The increased level of blood sugar in diabetes affects the whole body, not just the blood. “Elevated blood sugars appear in the mucus of the vagina and vulva, so they serve as an excellent culture medium for yeast,” says Daniel Einhorn, MD, vice president of the American Association of Clinical Endocrinologists. Yeast gets energy from sugar. So in an environment that is moist with sugar, yeast may overgrow.
Type 2 Diabetes: Diabetes and the Ability to Fight Yeast Infections
The effects of diabetes on the body becomes more obvious as time goes on. People who don’t keep good control of their blood sugar may develop complications related to the constantly high levels. One complication is difficulty in fighting off infections, either bacterial or fungal.
Dr. Einhorn explains, “Some women, especially those with poorly controlled diabetes, have some compromise in their ability to fight off any infection.” This means that once a yeast infection has begun, getting rid of it may not be that easy.
Type 2 Diabetes: Yeast Infection Treatment
Treatment of a yeast infection is the same for people with, or without, diabetes. “These infections are managed the [same] way as any other yeast infection. All the standard agents will work,” says Einhorn.
Over-the-counter treatments consist of antifungal vaginal creams and suppositories, which are used for one to seven days, depending on the product. Your doctor can tell you which product is best for you.
If your yeast infections are very frequent or don’t completely go away, your doctor may treat you for longer periods of time or prescribe a yeast infection medication called fluconazole. This is an effective treatment for yeast infection, but it shouldn’t be used if you’re pregnant.
Although most women believe they can tell if they have a yeast infection, this isn’t always the case. According to the Centers for Disease Control and Prevention, many women often misdiagnose themselves and buy over-the-counter yeast infection treatments that are ineffective for their problem. This is dangerous because the real problem is not getting properly treated. If you are uncertain if you have a yeast infection, or if your symptoms don’t go away with over-the-counter treatment, see your doctor for proper diagnosis and treatment.
Type 2 Diabetes: Lowering Your Risk of Yeast Infections
While yeast infections can’t always be prevented, you can lower your risk of developing one even if you have type 2 diabetes. Some tips that may help prevent yeast infections include:
- Avoid wearing tight-fitting clothes.
- Wear cotton underwear.
- Eat yogurt with live cultures of Lactobacillus acidophilus.
However, notes Einhorn, “The most important [way to prevent yeast infections] is to optimize glucose control so that the sugar in the secretions from the vulva and vagina doesn’t promote the buildup of glucose.”